Section Editors: Ivy Cheng, Alecs Chochinov
Adapting and Evolving in a Changing World
To adapt to a changing world, emergency care systems must continually improve their approach to creating, implementing, and integrating knowledge, within and beyond medicine.
Overview
Chapter 9: Just as we have made recommendations for clinical care, we begin with an exploration of integrating EM research into a broader system. This underlines the importance of tailoring research efforts to the biggest threats to our patients, populations, and planetary health.
Chapter 10: This chapter examines digital health (DH), addressing the potential of new technologies to transform how we communicate with each other, and care for patients virtually. The challenge for us is one of leadership and stewardship, to ensure that DH’s vast potential is realized in a cost-effective way that puts meaningful patient outcomes first and doesn’t drain valuable human resources from our EDs.
Chapter 11: Conflict and differing perspectives are major barriers to collaboration in service of the Quintuple Aim, especially in the ED. Sometimes differing perspectives appear inexplicable, leaving ED care providers frustrated and morally distressed. This chapter, entitled Managing Intergroup Relations, explains that understanding group dynamics and social identity are keys to moving out of our siloed past and collectively achieving better outcomes for patients.
Chapter 12: The EM:POWER project is a prime example of emergency medicine’s potential role in health policy and public affairs. In this chapter, the metaphor of the ED as the passive canary in the coal mine of health system dysfunction is challenged, and replaced with a more empowered construct, in which EM is a leading agent of change.
Chapter 13: Climate change is arguably the biggest health threat of the 21st century; yet many of us have an inadequate understanding of its impact on our patients and health system. This chapter includes a series of recommendations on how as physicians with expert knowledge and global responsibilities, we can prepare ourselves and our EDs for the impact of climate instability, mitigate the effects on our patients, and educate others.
Chapter 14: Boasting the acronym JEDI (not the Star Wars version) this chapter takes us full circle to the core values and principles that must guide us through an uncertain future. It outlines the challenges facing marginalized populations in the ED, with recommendations that focus on achieving a broader understanding of our diverse populations and equitable emergency care for all patients.
Chapter 15: This section ends with an exploration of healthcare strategies and lessons from other countries with liberal democratic values but different health systems. In an increasingly integrated world—and with the health of our patients at stake—it promotes the goal of becoming a true Learning Health System in which we use global knowledge and experience to continually improve.
Chapter 9: Coevolving in the Research and Quality Ecosystem
|
Over 20 years ago, Bégin et al criticized Canada’s fragmented healthcare system, [1] and described it as “a country of pilot projects.”. Proven innovations were rarely implemented, funded, or sustained, resulting in wasted investment, time, and effort. Unfortunately, the same can be said about Canada’s health research infrastructure, as revealed during the COVID-19 pandemic. At the time, many Canadian researchers looked on enviously as the UK’s National Institute for Health and Care Research (NIHR), among others, rapidly pivoted to launch pragmatic trials among Britain’s hospitalized COVID-19 patients. [2]
Within four months of the World Health Organization declaring a pandemic, the NIHR had completed and was reporting preliminary results from the RECOVERY Trial. [3] It determined that dexamethasone reduced 28-day mortality in patients with severe COVID-19. [4] Enabling and funding multicentre trials of the highest calibre rapidly changed practice and recommendations, with an immediate effect on clinical practice in Canada.
RECOVERY’s success was due to a pre-existing research network, the NIHR. In 2006, the UK government created the institute with a mission to support the National Health Service by enabling researchers to conduct cutting-edge research that focused on patient and population needs. [2] The NIHR can pivot its network quickly to focus on a single research question once it passes peer review. When COVID-19 was declared a pandemic, the NIHR simultaneously and rapidly provided funding, data sharing, privacy agreements, national harmonized ethics approval, clinical care and consent for its 176 members to begin the mammoth task of mounting this large-scale trial. [5]
More research networks are being established internationally. For example, the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) facilitates clinical trial operations, such as adaptive platform trials, and creates generic protocols like the WHO Clinical Characterisation Protocol. ISARIC’s goal is to create an international infrastructure that can efficiently keep up with the volume of knowledge required during a pandemic of a novel pathogen. This consortium produced the SOLIDARITY trial that globally evaluated interventions to treat COVID-19. [6]
These large multi-national networks likely saved hundreds of thousands of lives during the pandemic. By comparison, Canada lacked sustained research relationships, funding, infrastructure; [7] an efficient nationally harmonized ethics review process; uniform institutional privacy; and legal reviews. There were no flexible, pre-existing data-sharing agreements between the provinces or across the country. If this infrastructure had been available pre-pandemic, we could have rapidly accessed the real-time provincial data needed to accelerate pandemic research that would have provided comprehensive clinical or vaccine coverage information. [8] Further exacerbating our challenges was the emergency medicine workforce shortfall; in addition, the low numbers of Canadian researchers disproportionately impacted research.
Canada simply lacked the efficient processes or infrastructure to fund, launch and rapidly conduct multi-centre observational studies or trials. As a result, many researchers were unable to collect data at the speed necessary for timely clinical and policy decisions. Nor could they easily embed randomized control trials into routine clinical care, the way the NIHR could. [5] Consequently, Canada’s COVID-19 research output was frustratingly slow and lacked impact.
The 2021 commentary by Lamontagne et al. in the Canadian Medical Association Journal echoed the same problems as Bégin et al. had outlined two decades earlier: Canadian research infrastructure is still inefficient, culturally separate from clinical medicine, and fragmented. [9]
This needs to change.
As mentioned in other sections of this report, more investment and mentorship are required to increase the physician per capita ratio. This includes researchers. To avoid the fragmentation of a myriad of small, local topic-based research groups with limited capacity and sustainability, we must develop a pan-Canadian EM network with highly connected provincial (or geographic) nodes. Each should have the resources necessary to coordinate researchers across the EM spectrum, and facilitate inter-specialty, interdisciplinary and interprovincial collaborations. A fully-integrated research network would incorporate all stakeholders, including patients, knowledge users and government, so we can become a community of practice and learning health system.
The pandemic gave us pause for reflection. Shojania asked: “What problems in healthcare quality should we target as the world burns around us?” [10] Although the COVID-19 pandemic was the most widely recognized and urgent healthcare crisis, climate change, [11] the toxic drug crisis, [12] inequality, and systemic racism also require urgent attention through high-quality research and quality improvement. However, as Shojania points out, investment and effort continue to be spent on quality improvement projects and practice guidelines that have minimal outcome. [13][14] He consequently calls for change, and asks that efforts and funding be focused on the most urgent and impactful healthcare issues.
Emergency medicine faces many of the same questions: how can quality improvement and emergency medicine research evolve in our changing healthcare system to address the most urgent needs?
There is growing concern that traditional randomized controlled trials use exclusion criteria that are not applicable to the real-life, complex, and heterogeneous populations that are seen in our Emergency Departments. [15] Trials in Canadian emergency medicine have often limited recruitment to academic sites in urban areas, including those where researchers have personal connections. [16] This may have led to short-changing patients who have waited many years for the delayed results to become available, and in the meantime their well-being was impacted, with lives possibly lost.
Canadian emergency medicine research does, however, have a strong track record in conducting multi-centre cohort studies, [17][18][16][19][20] and the recent development of a pan-Canadian research network in Emergency Medicine, the Canadian COVID-19 Emergency Department Rapid Response Network (CCEDRRN), [21] (set up by NCER, the Network of Canadian Emergency Researchers) [22] builds on this. CCEDRRN has the potential to enable rapid and more efficient implementation of studies across the country, including adaptive trials that offer the potential for us to identify the best treatment for a given health problem.
According to Lamontagne et al., improving Canadian research will require small steps, avoiding traps by using thoughtful design, performing baseline evaluations with benchmarking, evaluating the return on investment, and conducting dialogue with political stakeholders. [9] The CIHR-IHPSR (Canadian Institutes of Health Research – Institute of Health Services and Policy Research) is incorporating these changes by introducing the learning health system (LHS) framework with a community of practice. [23] The LHS connects researchers, healthcare providers, patients, and communities to improve the most relevant healthcare issue. By adopting quality improvement methods, it uses Plan-Do-Study-Act (PDSA) cycles, baseline evaluations and benchmarks to foster continual improvement. [24] British Columbia’s emergency medicine community is re-organizing to become Emergency Care BC (ECBC), an LHS with a knowledge translation network that aims to implement new insights from research and quality improvement. [25]
Canada is developing big data platforms, an essential LHS building block [15] linked to digital health records, which includes external sources outside the healthcare system. In 2020, the Health Data Research Network Canada (HDRN) was created with the mission to use Canadian data to drive improvements in health and health equity. [26] HDRN is made up of 20 Canadian members who represent provincial, territorial, and national organizations with health data holdings. These are comprised of patient-orientated research unit data platforms [27] that can be used by researchers, policymakers and decision-makers. The barriers to rapidly and efficiently accessing multi-jurisdictional data are diminishing but will take time to overcome; yet HDRN is a critical piece of the much-needed pan-Canadian research infrastructure.
Researchers have historically worked in silos, but emergency medicine culture is changing rapidly. Canada’s pandemic-driven research networks include CCEDRRN, NCER, the Long COVID Web, and the Emerging and Pandemic Infections Consortium [28] (one of five national hubs awarded through the Canada Biomedical Research Fund by the Government of Canada), [29][30] Aligned with the Quintuple Aim, [31] emergency medicine research is emphasizing patient-orientated outcomes. [32] In addition to patients, these research collaborations extend across multiple disciplines, methods, and stakeholders, knowledge users, and government. Inspired by the achievements in the UK, resources need extending to expedited, nationally-harmonized ethics review, together with simplified privacy and legal approvals of research studies that include trials. This will require long-term government investment, and further development is needed to ensure sustainable funding.
Emergency medicine research is well-poised to contribute to learning health systems.
Recommendations: Coevolving in the Research & Quality Ecosystem
- Increase funding, training, infrastructure, and planning to support and expand the emergency medicine research workforce.
- Develop a pan-Canadian EM research network with highly connected nodes. Each node should have the resources necessary to coordinate researchers across the EM spectrum and facilitate inter-specialty, interdisciplinary and interprovincial collaborations. This network should incorporate all relevant stakeholders, so we can become an integrated community of practice and learning health system with a focus on achieving the Quintuple Aim.
- Facilitate data-sharing across jurisdictions. Develop a simplified and harmonized national approach to funding, data-sharing, privacy and legal agreements, ethics approval and research consent. Eliminate the need for redundant data, ethics, and privacy processes for multicentre and multi-jurisdictional research.
- Link clinical care, quality improvement, knowledge transfer and knowledge translation using models to move research rapidly to the bedside.
- Emergency medicine research efforts and funding should focus on the most urgent and impactful patient and population healthcare needs.
References
- Bégin M, Eggertson L, Macdonald N. A country of perpetual pilot projects. 2009.
- National Institute for Health and Care Research. National Institute for Health and Care Research.
- Horby P. Dexamethasone for COVID-19: preliminary findings. medRxiv. 2020 Jun;
- RECOVERY CG, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021 Feb 25;384(8):693–704.
- Murthy S, Fowler RA, Laupacis A. How Canada can better embed randomized trials into clinical care. 2020.
- ISARIC clinical characterisation group. Global outbreak research: harmony not hegemony. Lancet Infect Dis. 2020 Jul;20(7):770–2.
- Hohl CM, McRae AD. Antiviral treatment for COVID-19: ensuring evidence is applicable to current circumstances. CMAJ. 2022 Jul 25;194(28):E996–7.
- McRae AD, Archambault P, Fok P, Wiemer H, Morrison LJ, Herder M, et al. Reducing barriers to accessing administrative data on SARS-CoV-2 vaccination for research. CMAJ. 2022 Jul 18;194(27):E943–7.
- Lamontagne F, Rowan KM, Guyatt G. Integrating research into clinical practice: challenges and solutions for Canada. CMAJ. 2021 Jan 25;193(4):E127–31.
- Shojania KG. What problems in health care quality should we target as the world burns around us. CMAJ. 2022 Feb 28;194(8):E311–2.
- British Columbia Coroners Service. Heat-Related Deaths in B.C Knowledge Update. 2021 Nov 1;
- BC Gov News – Public Safety and Solicitor General. Toxic-drug supply cliams nearly 2,300 lives in 2022: BC Coroners Service. 2023 Jan 31;
- Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ. 1995 Nov 15;153(10):1423–31.
- Kwan JL, Lo L, Ferguson J, Goldberg H, Diaz-Martinez JP, Tomlinson G, et al. Computerised clinical decision support systems and absolute improvements in care: meta-analysis of controlled clinical trials. BMJ. 2020 Sep 17;370:m3216.
- Foley T. FF. The Potential of Learning Healthcare Systems. 2015 Nov;
- Stiell IG, Sivilotti MLA, Taljaard M, Birnie D, Vadeboncoeur A, Hohl CM, et al. Electrical versus pharmacological cardioversion for emergency department patients with acute atrial fibrillation (RAFF2): a partial factorial randomised trial. Lancet. 2020 Feb 1;395(10221):339–49.
- Stiell IG, Clement CM, Grimshaw J, Brison RJ, Rowe BH, Schull MJ, et al. Implementation of the Canadian C-Spine Rule: prospective 12 centre cluster randomised trial. BMJ. 2009 Oct 29;339:b4146.
- Stiell IG, Nichol G, Leroux BG, Rea TD, Ornato JP, Powell J, et al. Early versus later rhythm analysis in patients with out-of-hospital cardiac arrest. N Engl J Med. 2011 Sep 1;365(9):787–97.
- Perry JJ, Sivilotti MLA, Émond M, Stiell IG, Stotts G, Lee J, et al. Prospective validation of Canadian TIA Score and comparison with ABCD2 and ABCD2i for subsequent stroke risk after transient ischaemic attack: multicentre prospective cohort study. BMJ. 2021 Feb 4;372:n49.
- Thiruganasambandamoorthy V, Sivilotti MLA, Le Sage N, Yan JW, Huang P, Hegdekar M, et al. Multicenter Emergency Department Validation of the Canadian Syncope Risk Score. JAMA Intern Med. 2020 May 1;180(5):737–44.
- Canadian COVID-19 Emergency Department Rapid Response Network (CCEDRRN). [Internet]. 2023 [cited 2023 Feb 6]. Available from: https://www.ccedrrn.com/
- NCER | Better collaboration. Better research. Better care. [Internet]. [cited 2023 Aug 3]. Available from: https://ncer.ca/
- Canadian Institutes of Health Research. CIHR Institute of Health Services and Policy Research Strategic Plan 2015-19.
- Healthy Debate. Understand the Learning Health System.
- BC Emergency Medicine Network. BC Emergency Medicine Network Innovation Program.
- Health Data Research Network Canada. Health Data Research Network Canada.
- Canadian Institutes of Health Research. SPOR SUPPORT Units.
- University of Toronto. EPIC: Emerging and Pandemic Infections Consortium.
- Government of Canada. Award Recipients: Canada Biomedical Research Fund – Stage 1.
- Long COVID Web. Long COVID Web.
- Nundy S, Cooper LA, Mate KS. The Quintuple Aim for Health Care Improvement: A New Imperative to Advance Health Equity. JAMA. 2022 Feb 8;327(6):521–2.
- Archambault PM, McGavin C, Dainty KN, McLeod SL, Vaillancourt C, Lee JS, et al. Recommendations for patient engagement in patient-oriented emergency medicine research. CJEM. 2018 May;20(3):435–42.
Chapter 10: The Future of Digital Health in Emergency Medicine
There are no quick solutions to fixing Canada’s emergency care systems. The reality is that pre- pandemic, our EDs were already overcrowded, patients waited too long, and staff suffered from work stress. [1] Our efforts should not be directed towards turning the clock back to pre- pandemic conditions; rather, we should be focused on developing and implementing a blueprint for our ideal vision of Canada’s future emergency care.
The challenge of getting to that state from where we are is reminiscent of the lost tourist driving through rural Ireland who, when he comes across a farmer in a field, stops and asks him how to get to Dublin. The farmer thinks for a moment and replies, “Going to Dublin, are ya? I would not start from here.” Like the traveller, our starting place may not be the one we choose but is where we are.
There are a few key attributes of a better emergency care system we can work towards. One is meaningful horizontal integration with the rest of the healthcare system, especially primary care and community-based services. Too often in the ED we fly blind, with limited access to a patient’s medical history, care providers and prior investigations. Lacking the information to choose wisely, we choose safely, often ordering tests that would not otherwise be necessary. Similarly, our ability to connect patients for needed care or follow-up after ED discharge is often limited to ‘hope-and-a-prayer’ faxes, transmitted to clinics that may or may not agree to see the patient at some uncertain time in the future.
It is critical to ensure primary care and hospital records are available as part of a shared provincial electronic health record (EHR). [2] Better information sharing could also enable more cost-effective virtual emergency care. In some provinces today, the EHR—if it exists at all—consists only of a viewer with a somewhat random and incomplete collection of records in non-standard formats and timeliness. Accountability to populate EHR systems is also lacking: why not make payment for any publicly-funded healthcare service conditional on the real-time uploading of the clinical record to the EHR in a standard format?
A more integrated digital emergency care system will allow an actual appointment, with a date and time to be booked before the patient leaves the ED. Better yet why not have the patient book it themselves, at a time of their choosing? Such certainty gives both ED provider and patient peace of mind. It can also enable the physician to be more circumspect in ED investigations, knowing there will be a timely follow-up.
Giving patients access to their own health data (which increasingly patients are considered to own) will empower them, give them more control, the ability to manage their care, and help improve outcomes. [2] Access does not need to be one way; patients could also enter their own health data (such as biophysical measurements from wearables), [3] report their symptoms, [4], and outcome measures, [5], which are critical to understanding the important results of ED care.
Finally, we must consider whether those we think of as ‘lost ED tourists’ do not see themselves that way. While some patients would almost certainly seek care elsewhere if alternatives were available and accessible, many others decide to go to the emergency department simply because they believe they need care there. [6] The ED provides a one-stop shop for medical assessment, labs tests, imaging, treatment, and consultation with specialists if needed.[10] Many patients know through personal experience that if they look for care elsewhere, they will likely be sent to the ER anyway. Efforts to focus on ‘real’ emergencies by limiting ED access for so-called inappropriate patients may be destined to fail. [7] Societal expectations may be partly at play; many patients today are used to getting what they need when they need it in the most convenient way (think Amazon, Uber Eats or online banking). The ED as a one-stop-shop may be the health system’s version to this phenomenon. Rather than devising strategies to reverse these trends, like generals planning to fight the last war, perhaps we need to embrace the fact that today’s patients are voting with their feet, and plan accordingly.
This requires re-imagining EDs and building the necessary digital integration with primary and community care. The answer lies in an integrated care network with:
- Improved supports for older persons with frailty.
- Better mental health, addiction, and social services.
- Enhanced access to 24/7 diagnostic testing.
- A full suite of follow-up clinic and services accessible in the ED.
Although this may seem overly optimistic, the truth is innovative examples are increasingly found in our system but remain a patchwork. These range from EDs designed with specific supports for geriatric care, [8][9] pathways for rapid low-barrier access to addiction services, [10] and homeless shelter services integrated with EMS. [11] They must be scaled up and properly funded, with adequately trained members of a diverse healthcare team.
In this journey of health system transformation, all of us—patients and providers alike—are lost travelers, and it’s a long way to Dublin. If we are ever to find our way, we must envision and then build an innovative and integrated future state for emergency care together, using all the tools at our disposal.
Introduction
This chapter aims to map out the current landscape of Digital Health (DH) and Virtual Care (VC) in emergency medicine, identify opportunities and areas of concern, and propose a roadmap where these tools can be effectively embraced as integral parts of our discipline. We take it as self-evident that Canada should continue to advance the meaningful use and adoption of interoperable electronic health records. They enable healthcare providers to access and exchange patient data easily, even between different EHR platforms. For example, computerized provider order entry, where patient data is recorded electronically, allows doctors and healthcare providers to manage care orders such as prescriptions, tests, or treatments.
Below, we focus on VC as well as some emerging technologies that could make a valuable contribution to emergency care.
The Pros and Cons of Digital Health and Virtual Care
Digital Health (DH) encompasses a rapidly advancing collection of technology-enabled tools to improve access to healthcare services and information. The Health Information and Management Systems Society (HIMSS) states that, “Digital health connects and empowers people and populations to manage health and wellness, augmented by accessible and supportive provider teams working within . . . digitally-enabled care environments that strategically leverage digital tools, technologies and services to transform care delivery.” [12]
The World Health Organization (WHO) identifies three key objectives in adopting and scaling up DH to “accelerate global attainment of health and wellbeing”: [13]
- Translating the latest data, research, and evidence into action.
- Enhancing knowledge through scientific communities of practice.
- Systematically assessing and linking country needs with supply of innovations.
Emergency medicine can capably contribute to all three objectives through health services research and implementation in urgent and emergency care domains.
While the potential for DH to transform healthcare has been recognized for several decades, the pandemic precipitated its rapid and massive clinical adoption through Virtual Care services and remote patient monitoring. [14] These practices facilitated the delivery of services, while maintaining social isolation to avoid viral transmission, in compliance with public health policies. The rapidity of DH adoption led to both opportunities [15] and challenges [16] for emergency medicine.
On the one hand, appropriate use of DH and VC can potentially reduce emergency department surges, overcrowding and long wait times. It can provide support and knowledge exchange with colleagues practicing in rural communities, as well as supporting safe discharge and patient self-management through remote monitoring.
On the other hand, flawed design and implementation can result in paradoxical overcrowding of EDs through poor VC case management by health professionals who unnecessarily send patients to the emergency for care. Additionally, VC’s attractive practice and compensation models can draw emergency physicians away from the ED where they are most needed.
It’s essential to purposefully integrate these approaches with traditional emergency medicine service delivery; they can maximize patient safety and convenience, and provide value to the healthcare system. Working towards a future of hybrid care [17] that fulfills the Quintuple Aim will preclude the need to choose between VC or in-person care, but rather encourage the thoughtful combination of both to optimize emergency health service delivery and transform our specialty. [18]
How Can Digital Health Creatively Support EM?
VC is the best-known and most widely used type of digital health in emergency medicine. COVID-19 provided the impetus for many hospital-led VC programs across the country. Their adoption aimed to preserve the healthcare system’s scarce in-person resources, while increasing access to care. Some EDs in Ontario began offering a virtual ED for patients with urgent, but non-life-threatening concerns.
Prior to the pandemic, other emergency VC services included telemedicine to support prehospital care. [19] Patients in BC and Alberta who contacted 811 were triaged by a nurse to attend an ED, and instead were assessed virtually by an emergency physician. The preliminary results were promising, with such physicians safely and cost-effectively diverting a significant number of patients away from the emergency department. [20][21]
Post-pandemic, EDs face overcrowding and long wait times. [22][23] VC can mitigate this, as evidenced by British Columbia’s HEiDi project, which resulted in high patient satisfaction and ED avoidance in lower acuity cases. [20] DH is especially beneficial for healthcare providers if VC is accessed with provincial health records; this offers seamless communication with primary care, along with more transparent and efficient prescribing of diagnostics and therapies.
Patients who need emergency care can benefit from home monitoring and wearable technologies which can be divided into out-of-hospital and in-hospital devices. In the community, these can be paired with smartphone apps that can detect chronic deteriorating health conditions, such as rhythm changes in patients with atrial fibrillation, track changes in spirometry (breathing capacity) in those with lung disease, [24][25] and measure adherence to oral medications. [24] Monitoring medications after discharge from an ED can help patients recovering from acute injury, tracking opioid use for example. [26] Other wearables are specifically designed to act as an overall health safety net, capable of tracking and automatically alerting family and/or healthcare providers about changes in vital signs, and potential falls. [27] In hospital, wearables can monitor patient vital signs, and remote telemetry can gather real-time information on patients who are not in a physical space with monitors. [28] Given worsening crowding problems in Canada’s EDs, this could be particularly beneficial.
In the future, machine learning (ML) and artificial intelligence (AI) will play important roles in the ED. While the black box of AI functionality, privacy and medical liability need to be addressed, there is no doubt it can lessen cognitive load and stress by adding a level of predictive modelling to medical decision-making for physicians. [29-31] AI has demonstrated promise in helping to interpret diagnostic imaging and predicting fatal infections like sepsis. It has also been able to assess patients who may suffer a lack of blood flow to the brain and might be at risk of a future cardiac event. Recent leaps in large language processing, such as ChatGPT, suggest AI’s added potential to help provide detailed medical records based on short instructions, without providers having to create a template.
The Challenges of Incorporating DH and VC into Emergency Medicine
|
VC in medicine is well over a century old, [32] and remote communities in Canada have used it to help treat emergency patients well before the COVID-19 pandemic. Nevertheless, there are ongoing challenges that must be addressed, including:
- Data security concerns and privacy.
- Limited physical exam options.
- Health equity concerns, for example the risk of alienating vulnerable groups due to technology and access issues. The homeless, older persons and new immigrant populations are prime examples.
- The perception among many emergency physicians that virtual visits have increased ED visits. A recent study by Kiran et al demonstrated that physicians with a high proportion of VC did not have higher ED visits for their patients than those who provided the lowest levels of virtual care. [33] Further study, addressing the full spectrum of ED-UC VC, is needed.
- Workforce issues, including those in which the limited resource of emergency physicians is drawn to less onerous, but less essential work in certain VC settings
- The loss of in-person care, which could adversely affect the culture of emergency medicine and the benefits accrued from face-to-face care contact between doctor and patient.
The Canadian Medical Protective Association (CMPA) has set out the following additional challenges that must be considered when providing VC: [34]
- Risk of exacerbating the fragmented approach to healthcare across Canada.
- Inconsistency in standards and guidelines regarding when it is reasonable to use virtual care.
- Lack of proper infrastructure and training on the various modalities of virtual care.
- Lack of access to secure virtual care platforms.
A major concern is the private involvement in DH development. While innovation is welcome and fuelled by entrepreneurship, careful guardrails are needed to ensure that private interest does not influence the processes or privacy of care. [35,36] Precious resources must be focused on safe public delivery of ED care—and not on DH privatization.
Visioning the Future with Digital Emergency Medicine
The need for emergency medical services continues to rise, resulting in a shortage of resources and an overwhelming workload for EM practitioners. The situation has been extensively described elsewhere in this report overcrowded EDs, long wait times, and limited availability of essential supplies and equipment. DH includes a set of invaluable tools to help emergency care systems scale up services, improve patient outcomes, reduce mortality and morbidity, and better manage data to deliver healthcare. [37] DH must not replace in-person care, with its attendant tangible and intangible benefits, but can augment and complement its overall provision.
DH should also be considered an adjunct to human resources. ED staff can actively participate to integrate and implement DH into the clinical workflow by identifying the “why, what, how” of DH projects and prioritize them in specific purposes. ED leaders are encouraged to participate in DH research and implementation in an integrated manner within the community healthcare system (hospital, primary care, mental health program, etc.) as well as within provincial, national, and international networks.
Conclusion
Digital and technological innovations are scaling rapidly, and medicine continues to adopt and implement the best of them into every specialty. In a future not too far from now, DH will transform medicine. Metabolomic (the study of small molecules in a cell or tissue) and genomic (gene-related) findings mean treatments can be customized to a person’s genetic makeup. This will change the way we treat patients, choose and tailor pain medications, antibiotics, or anti-depressants for instance. AI will accelerate notetaking and prescribing, [38] as well as helping to monitor patients, and detect diseases in early stages. These areas of research will open doors to personalized diagnostics and treatment. Emergency medicine leaders must be proactive by integrating these technologies to enable the best possible patient outcomes.
DH is an inevitability in emergency care. The question is not whether DH will be adopted, but rather how technology can help forge a path to achieve the Quintuple Aim of improved patient experience, better population outcomes, lower costs, an empowered workforce, and health equity for all Canadians. The latter two are worth reiterating: if DH proves a burden to providers, and inaccessible to our most vulnerable, this technological revolution will be met with resistance rather than acceptance. It’s therefore imperative to understand both the vast potential and the pitfalls of DH, so we can choose future applications and resource allocations wisely.
Recommendations for Digital Health in the EM
- EM leaders in Canada must work together with all stakeholders to build a DH record system which allows access for both patients and direct healthcare providers.
- To achieve this, health information systems should be integrated at regional, as well as F/P/T levels.
- Emergency physicians must embrace leadership and stewardship roles in DH, to ensure that the most effective initiatives are supported and that precious public resources are not diverted to frivolous ventures or privatization of DH.
- EM specialists should assume key roles in the regulation of DH applications in healthcare by way of legislation and government policies.
- Departments of EM and EM professional societies should collaborate in national and global translational (practically-oriented) research to best apply digital heath’s strengths to EM’s needs.
- EM training and professional development should be reviewed to ensure core competencies related to the use of DH are taught.
- Digital health should be a focus of quality improvement initiatives at hospital EDs and academic ED departments.
- Appropriate consideration should be given to the varying levels of digital literacy, access, and education in Canada’s populations to help prevent barriers to the equitable and fair implementation of digital ED health. [39,40]
References
- News · CBC. CBC. 2019 [cited 2023 Sep 6]. Wait times at Ontario hospitals climbed to record high this summer, data shows | CBC News. Available from: https://www.cbc.ca/news/canada/toronto/june-hallway-medicine-data-1.5271281
- Tapuria A, Porat T, Kalra D, Dsouza G, Xiaohui S, Curcin V. Impact of patient access to their electronic health record: systematic review. Inform Health Soc Care. 2021 Jun 2;46(2):192–204.
- Dinh-Le C, Chuang R, Chokshi S, Mann D. Wearable Health Technology and Electronic Health Record Integration: Scoping Review and Future Directions. JMIR Mhealth Uhealth. 2019 Sep 11;7(9):e12861.
- Cancer Care Ontario [Internet]. 2017 [cited 2023 Sep 6]. Patient Reported Outcomes & Symptom Management Program. Available from: https://www.cancercareontario.ca/en/cancer-care-ontario/programs/clinical-services/patient-reported-outcomes-symptom-management
- Vaillancourt S, Cullen JD, Dainty KN, Inrig T, Laupacis A, Linton D, et al. PROM-ED: Development and Testing of a Patient-Reported Outcome Measure for Emergency Department Patients Who Are Discharged Home. Ann Emerg Med. 2020 Aug;76(2):219–29.
- Vogel JA, Rising KL, Jones J, Bowden ML, Ginde AA, Havranek EP. Reasons Patients Choose the Emergency Department over Primary Care: a Qualitative Metasynthesis. J Gen Intern Med. 2019 Nov;34(11):2610–9.
- Atkinson P, McGeorge K, Innes G. Saving emergency medicine: is less more? CJEM. 2022 Jan;24(1):9–11.
- News · CBC. CBC. 2022 [cited 2023 Sep 6]. Why a first-of-its-kind seniors emergency care centre could be an important test for Ontario | CBC News. Available from: https://www.cbc.ca/news/canada/toronto/seniors-emergency-care-centre-toronto-western-hospital-1.6685550
- Vermond K. Your Health Matters. 2020 [cited 2023 Sep 6]. ED One Team fights “hallway medicine.” Available from: https://health.sunnybrook.ca/magazine/sunnybrook-magazine-fall-2020/ed-one-team-hallway-medicine/
- Rapid Access Addiction Medicine Clinic – Addiction Services – Toronto – Sunnybrook Hospital [Internet]. [cited 2023 Sep 6]. Available from: https://sunnybrook.ca/content/?page=bsp-rapid-addiction-medicine
- Toronto [Internet]. 2022 [cited 2023 Sep 6]. New hospital program helps Toronto’s homeless, cuts ambulance offload time. Available from: https://toronto.ctvnews.ca/new-hospital-program-helps-toronto-s-homeless-cuts-ambulance-offload-time-1.6209499
- MobiHealthNews [Internet]. 2020 [cited 2023 Sep 6]. HIMSS launches new definition of digital health. Available from: https://www.mobihealthnews.com/news/himss-launches-new-definition-digital-health
- Digital health [Internet]. [cited 2023 Sep 6]. Available from: https://www.who.int/health-topics/digital-health#tab=tab_1
- Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017 Oct 19;377(16):1585–92.
- Ho K. Virtual care in the ED: a game changer for the future of our specialty? CJEM. 2021;23(1):1–2.
- Innes G. Fast food medicine. Canadian Journal of Emergency Medicine. 2023;1–2.
- Licurse A, Fanning K, Laskowski K, Landman A. Balancing Virtual and In-Person Health Care. Harvard Business Review [Internet]. 2020 Nov 17 [cited 2023 Sep 6]; Available from: https://hbr.org/2020/11/balancing-virtual-and-in-person-health-care
- Disruptive and Sustaining Innovation in Telemedicine: A Strategic Roadmap | NEJM Catalyst [Internet]. [cited 2023 Sep 6]. Available from: https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0311
- Amadi-Obi A, Gilligan P, Owens N, O’Donnell C. Telemedicine in pre-hospital care: a review of telemedicine applications in the pre-hospital environment. Int J Emerg Med. 2014 Jul 5;7:29.
- Ho K, Lauscher HN, Stewart K, Abu-Laban RB, Scheuermeyer F, Grafstein E, et al. Integration of virtual physician visits into a provincial 8-1-1 health information telephone service during the COVID-19 pandemic: a descriptive study of HealthLink BC Emergency iDoctor-in-assistance (HEiDi). Canadian Medical Association Open Access Journal. 2021 Apr 1;9(2):E635–41.
- Services AH. Alberta Health Services. [cited 2023 Sep 6]. Virtual MD connects Health Link callers directly to physicians. Available from: https://www.albertahealthservices.ca/news/Page16756.aspx
- Huffman A. From “A Campfire to a Forest Fire”: The Devastating Effect of Wait Times, Wall Times and Emergency Department Boarding on Treatment Metrics. Annals of Emergency Medicine. 2023 Jan 1;81(1):A13–7.
- Kenny JF, Chang BC, Hemmert KC. Factors Affecting Emergency Department Crowding. Emergency Medicine Clinics of North America. 2020 Aug 1;38(3):573–87.
- Chai PR, Carreiro S, Innes BJ, Chapman B, Schreiber KL, Edwards RR, et al. Oxycodone Ingestion Patterns in Acute Fracture Pain with Digital Pills. Anesth Analg. 2017 Dec;125(6):2105–12.
- Li T, Divatia S, McKittrick J, Moss J, Hijnen NM, Becker LB. A pilot study of respiratory rate derived from a wearable biosensor compared with capnography in emergency department patients. Open Access Emerg Med. 2019;11:103–8.
- Ho K, Novak Lauscher H, Cordeiro J, Hawkins N, Scheuermeyer F, Mitton C, et al. Testing the Feasibility of Sensor-Based Home Health Monitoring (TEC4Home) to Support the Convalescence of Patients With Heart Failure: Pre–Post Study. JMIR Form Res. 2021 Jun 3;5(6):e24509.
- Darwish A, Hassanien AE. Wearable and Implantable Wireless Sensor Network Solutions for Healthcare Monitoring. Sensors (Basel). 2011 May 26;11(6):5561–95.
- Miller K, Baugh CW, Chai PR, Hasdianda MA, Divatia S, Jambaulikar GD, et al. Deployment of a wearable biosensor system in the emergency department: a technical feasibility study. Proc Annu Hawaii Int Conf Syst Sci. 2021 Jan 5;2021:3567–72.
- Kirubarajan A, Taher A, Khan S, Masood S. Artificial intelligence in emergency medicine: A scoping review. Journal of the American College of Emergency Physicians Open. 2020;1(6):1691–702.
- Artificial intelligence and machine learning in emergency medicine: a narrative review – Mueller – 2022 – Acute Medicine & Surgery – Wiley Online Library [Internet]. [cited 2023 Sep 6]. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/ams2.740
- Grant K, McParland A, Mehta S, Ackery AD. Artificial Intelligence in Emergency Medicine: Surmountable Barriers With Revolutionary Potential. Ann Emerg Med. 2020 Jun;75(6):721–6.
- Aronson SH. The Lancet on the telephone 1876-1975. Med Hist. 1977 Jan;21(1):69–87.
- Kiran T, Green ME, Strauss R, Wu CF, Daneshvarfard M, Kopp A, et al. Virtual Care and Emergency Department Use During the COVID-19 Pandemic Among Patients of Family Physicians in Ontario, Canada. JAMA Netw Open. 2023 Apr 28;6(4):e239602.
- CMPA [Internet]. [cited 2023 Sep 6]. CMPA – White paper—Integrating virtual care in practice: Medico-legal considerations for safe medical care. Available from: https://www.cmpa-acpm.ca/en/research-policy/public-policy/integrating-virtual-care-in-practice–medico-legal-considerations-for-safe-medical-care
- Grande D, Luna Marti X, Feuerstein-Simon R, Merchant RM, Asch DA, Lewson A, et al. Health Policy and Privacy Challenges Associated With Digital Technology. JAMA Network Open. 2020 Jul 9;3(7):e208285.
- Horn R, Kerasidou A. Sharing whilst caring: solidarity and public trust in a data-driven healthcare system. BMC Medical Ethics. 2020 Nov 3;21(1):110.
- Abernethy A, Adams L, Barrett M, Bechtel C, Brennan P, Butte A, et al. The Promise of Digital Health: Then, Now, and the Future. NAM Perspect. 2022:10.31478/202206e.
- Choudhary G. mint. 2023 [cited 2023 Sep 6]. GPT-4 simplifies medical writing for prescriptions and notes. Know here’s how. Available from: https://www.livemint.com/technology/apps/gpt4-simplifies-medical-writing-for-prescriptions-and-notes-know-here-s-how-11679379420629.html
- Hyman A, Stacy E, Mohsin H, Atkinson K, Stewart K, Lauscher HN, et al. Barriers and Facilitators to Accessing Digital Health Tools Faced by South Asian Canadians in Surrey, British Columbia: Community-Based Participatory Action Exploration Using Photovoice. Journal of Medical Internet Research. 2022 Jan 13;24(1):e25863.
- Whitelaw S, Pellegrini DM, Mamas MA, Cowie M, Van Spall HGC. Barriers and facilitators of the uptake of digital health technology in cardiovascular care: a systematic scoping review. Eur Heart J Digit Health. 2021 Mar;2(1):62–74.
Chapter 11: Managing Intergroup Relations
Conflict among the programs, sites, professions, and specialties that provide care impairs how systems function, and prevents a shared vision for change from developing. Unfortunately, such conflict is pervasive in healthcare. [1] It certainly appears in the emergency department (ED), where a diffuse patient population and complex interconnections with other departments create prime conditions for strife about who “owns” which patient.
A classic study documented how ED patient charts—supposedly repositories of objective information—were battlegrounds of inter-specialty competition and sniping, with potentially devastating consequences for patients caught in the crossfire. [2] The picture is hardly prettier at the system level, with its ubiquitous silos among professions, programs, sites, and sectors, not to mention between clinicians and management. [3]
Why, then, are intergroup relations so problematic, and what can we do about it?
Getting to the Root Cause
To start with, this isn’t an interpersonal issue that can be solved by sending everyone for training in communication skills: the problem doesn’t reflect lack of skill, but rather the active expression of strongly-held social identities. [2] These are the parts of people’s identity that come from being a member of a group or category, such as one’s nationality, gender, profession, or department. While there are many formal and folk theories of how groups operate, social identity theory [4,5] outperforms with its comprehensiveness, theoretical coherence, and robust evidence base. [6] It provides a broad, multifaceted approach to understanding how people interact with others within and between groups.
Decades of research have illustrated the powerful force of social identity; even meaningless groups assigned in a lab can influence the way people treat in-group vs. out-group members. [4-6] In reality, of course, social identities are not empty labels, but include meaningful identity content (such as group-defining characteristics, norms, and values) which makes them all the more powerful. [7]
Why do we categorize ourselves and others? Doing so serves two deep needs: the cognitive need to simplify the social world, and the emotional need to identify with something greater than ourselves. [4,5] In other words, social identity isn’t going away. Nor should it. Although negative outcomes, such as prejudice, discrimination, and conflict come to mind, shared identity can also be the wellspring of collaboration, altruism, and solidarity. [8] The question is not how to get rid of social identities (we can’t) but how to manage them so that their effects are positive instead of negative.
The most obvious solution is to urge everyone to abandon narrow distinctions and transfer their identification to one all-encompassing group. After all, aren’t we all here for the patient? We see how when a crisis strikes, say, after a natural disaster, or at the height of the pandemic, everyone unites behind a common cause, putting aside intergroup rivalries—only to take them up again when the crisis abates. Why can’t we all simply identify as healthcare providers, or indeed, as members of humanity?
It’s not that simple. For one thing, we are wired to pay attention to intergroup contrast. [5] Under most circumstances, an abstract, all-inclusive category provides very little information about the social world. It also tends to have limited emotional resonance; it is hard to get excited about who we are if nothing distinguishes us from anyone else. All things being equal, groups with high distinctiveness (owing to their small size, unique identity content, and/or alignment with meaningful physical boundaries) are most likely to be significant to us, as observed both within and outside healthcare. [3,5] So although a crisis can temporarily override intergroup distinctions, we should not be surprised when they surface again.
Additionally, people react unfavourably to the prospect of a valued identity being removed or altered. [8] Unfortunately, identity threat, as it is called, can easily be triggered by well-meaning appeals to put aside intergroup differences in favour of the common good, [1.9] especially if they come from an outgroup. This is even more likely if the subtext is “we’d all get along if only you people would be more like us,” an appeal for unity that appears more often than you’d think. [10] But the problem cannot be remedied merely by crafting better messages: any perceived challenge to a valued group’s existence, status, distinctiveness, or norms—essentially any attempt to get people to work together differently—can trigger identity threat, and spark resistance.
So how can change ever succeed?
Strategies that Work
Change can take place by working through social identities, not against them. [1,6] A diverse body of literature has uncovered a sequence dubbed reinforce-redefine-replace. [10] Counterintuitive as it may seem, agents of change must start by reinforcing existing identities, reassuring members that the groups and group-defining values they cherish will not disappear. Once these identities are secure and not under threat, members may entertain ideas that somewhat redefine the group and/or its relationship to others, so long as a strong link to the past is retained. Eventually, a new conception of group identity, or of an intergroup relationship, may come to replace the old.
The literature offers diverse examples of reinforce-redefine-replace sequences, such as the following:
Building a Mosaic Identity
Several organizations struggling to improve staff engagement have found the ASPIRe (Actualizing Social and Personal Identity Resources) model [9] helpful. After a phase of discovering what sub-groups (e.g., profession, department) are locally meaningful, employees meet in identity-based subgroups (reinforce) before coming together to identify commonalities (redefine) and finally set shared goals (replace).
This process seeks to build a mosaic identity that recognizes each subgroup’s uniqueness as well as its contribution to a larger whole. Separate from tests of the ASPIRe model, the theme of mosaic identity has emerged strongly from case studies of organizations that have achieved a high degree of interprofessional collaboration, such as the Dana Farber Cancer Institute. [10]
Reinforcing Another Group’s Identity
Conflict between managers and physicians is common in healthcare, and many hospitals have tried to repair strained relationships. Leaders’ efforts often begin with overtures to reopen communication with physicians and build one-on-one relationships, but then what? The most effective next steps are typically those that reinforce physician identity, for instance by supporting their ability to act as a group. This might include encouraging the formation of a physician advisory board and compensating members for their time; upholding physician norms such as keeping meetings brisk and action-oriented; and using language that belongs in a clinical setting rather than a corporate boardroom. [12,13] Such actions can help advance the intergroup relationship to a point that allows cooperation around specific objectives (redefine), and eventually, the development of shared goals and structures (replace). However, this process cannot be forced or rushed. One hospital CEO, emboldened by the success of early efforts to de-escalate tension, decided to leapfrog over stages, and moved quickly to ask everyone to create a common agreement for working together. Conflict immediately flared again, and the CEO was back on the phone with the social identity consultant, who backed away slowly. [12] Even a smaller leap from interpersonal strategies to the redefine phase has shown evidence of backfiring. [11]
Honouring the Past
Back in the 1950s, nursing textbooks would praise Florence Nightingale as the physician’s loyal helper, a subservient role considered part of nursing identity. As the decades advanced, gender roles changed and nursing roles along with them, but the textbooks could not very well abandon their pioneer. So, they did not. They just let the idea of subservience quietly slip away, while focusing on aspects of nursing identity that did not change, such as being nurturing. The authors also began to introduce new aspects that were more consistent with equal status, such as patient advocacy, a commitment to holism, and eventually, the possession of a distinct body of scientific knowledge. And who did they position as the scientific, holistic patient advocate? You guessed it: Florence Nightingale. [14]
At no point did the textbooks explicitly break with the past; rather, they emphasized a sense of continuity with history to legitimize new features of this identity. A similar process over a shorter time frame is seen in studies of physicians who participate in new models of primary care. In this case, their identity shifts from autonomous expert to head of team by gradually incorporating new elements that are perceived as congruent with the old. [15]
Putting it Together
The literature also suggests that identity mobilization works in alternation with practical, concrete changes to the working environment. [1] The purpose of reinforcing and redefining identities is to build enough support to implement practical changes; once implemented, such change can stimulate further identity reshaping, enabling a more extensive shift in the next cycle.
Education and training are particularly important settings for social identity management. Interprofessional education programs have demonstrated positive impacts on both learners and patients and should continue to be expanded and refined. [16] It’s also crucial that residency programs include opportunities for productive interaction among specialties, for instance, by ensuring that internal medicine residents rotate through the ED. Collaborative experiences during the process of forming a person’s identity can promote identification with a group beyond one’s own profession or specialty, and at the same time establish teamwork as part of one’s professional identity.
This chapter has focused on managing the internal dynamics of the healthcare system. Of course, social identity theory has much broader applications. Better understanding of identity processes could enhance our efforts to combat racism in healthcare, and to promote EDI more generally. Social identity thinking may also help the health community engage more effectively with the public on health policy and public health issues.
Conclusion
There is no magic bullet when it comes to implementing system change: no matter how carefully social-identity-management strategies are selected and calibrated, the process remains difficult, and the outcome uncertain. Nonetheless, it can be helpful to block off time to examine potential strategies through this lens. Understanding how social identities work—in particular, the problem of identity threat and the promise of reinforce-redefine-replace sequences—can help change agents increase the chance of success.
References
- Kreindler SA, Dowd D, Star N, Gottschalk T. Silos and social identity: The social identity approach as a framework for understanding and overcoming divisions in healthcare. Milbank Q 2012; 90(2): 347- 374.
- Hewett DG, Watson BM, Gallois C, Ward M, Leggett BA. Communication in medical records: intergroup language and patient care. Journal of Language and Social Psychology; 2009; 28(2):119- 138.
- Kreindler SA, Hastings S, Mallinson S, Brierley M, Birney A, Tarraf R, Winters S, Johnson K. Managing intergroup silos to improve patient flow. Health Care Manage Rev 2022; 47(2): 125-132.
- Tajfel H, Turner JC. An integrative theory of intergroup conflict. In G. Austin, & S. Worchel (Eds.), The social psychology of intergroup relations (pp. 33-47). Monterey: Brooks/Cole; 1979.
- Turner JC, Hogg MA, Oakes PJ, Reicher SD, Wetherell MS. Rediscovering the social group: A self- categorization theory. Oxford: Blackwell; 1987.
- Haslam SA. Making good theory practical: Five lessons for an Applied Social Identity Approach to challenges of organizational, health, and clinical psychology. British Journal of Social Psychology 2014; 53(1): 1-20.
- Ellemers NE., Spears R., Branscombe NR. (Eds.). Social identity: context, commitment, content. Oxford: Blackwell; 1999.
- Ellemers N, Spears R, Doosje B. Self and Social Identity. Annual Review of Psychology 2002; 53, 161- 186.
- Haslam SA, Eggins RA, Reynolds KJ. The ASPIRe Model: Actualizing social and personal identity resources to enhance organizational outcomes. Journal of Occupational and Organizational Psychology 2003; 76: 83-113.
- Kreindler SA. The politics of patient-centred care. Health Expect 2015; 18(5): 1139-50
- Kreindler SA, Struthers A, Metge CJ, Charette C, Harlos K, Beaudin P, Bapuji SB, Botting I, Francois J. Pushing for partnership: Physician engagement and resistance in primary care renewal. J Health Org Manag 2019; 33(2): 126-140
- Fiol CM, Pratt MG, O’Connor EJ. Managing intractable identity conflicts. Academy of Management Review 2009; 34(1): 32-55.
- Kreindler SA, Larson BK, Wu FM, Gbemudu JN, Carluzzo KL, Struthers A, Van Citters AD, Shortell SM, Nelson EC, Fisher ES. The rules of engagement: Physician engagement strategies in intergroup contexts. J Health Org Manag 2014; 28(1): 41-61.
- Goodrick E, Reay T. Florence Nightingale endures: Legitimizing a new professional role identity. Journal of Management Studies 2010; 47(1): 55-84.
- Reay T, Goodrick E, Waldorff S, Casebeer A. Getting leopards to change their spots: co-creating a new professional role identity. Academy of Management Journal 2016; 60(3): 1043–1070.
- Reeves S, Fletcher S, Barr H, Birch I, Boet S, Davies N, McFayden A, Rivera J, Kitto S. A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39. Medical Teacher 2016; 38(7): 656-668. Emergency Medicine’s Future Role in Health Policy and Public Affairs.
Chapter 12: Emergency Medicine’s Future Role in Health Policy and Advocacy
|
Background
Emergency department closures and crowding, with their potential lethal consequences, are garnering media attention across the country. [2] Building on shared national goals, it makes sense to have a coordinated effort to address these issues, and that is the purpose of this report, clearly articulated in our overarching recommendations.
But it will take more than words—however well-intentioned and informed—to produce meaningful change. That is where engagement in policy, public affairs and advocacy begins.
Healthcare in Canada is largely under provincial jurisdiction. The Canada Health Act provides conditions for federal health transfers to the provinces for hospital and medical care, but each province organizes and operates its own system within the very broad parameters of the Act. [1] Despite regional differences, however, healthcare shortfalls are widespread across Canada and similar in nature from province to province.
The Role of the Emergency Department in a Dysfunctional Health System
EDs fulfill a unique but increasingly difficult role in the health system. Through the patients they see, emergency physicians are witness to a host of social and health system ills that give them unique insights into the system and its failings.
The oft-used metaphor of the ED as the canary in the coal mine [3] is unfortunate, as it paints a picture of emergency staff as passive and reactive. The EM:POWER message is that ED professionals have the agency, credibility, and experience to be proactive, because we work at a critical healthcare intersection, the junction between community, prehospital, primary, and acute care. We provide services ranging from resuscitation to public health to geriatrics. EDs are the decision point for most hospitalizations, a gateway to urgent imaging, surgery, specialty care and critical care.
We are the only open door for many complex and marginalized patients and for growing numbers of those unable to access the right care in the right place. ED providers have a unique system perspective, a view of many possible pathways, including promising future directions. In that new construct, emergency physicians can be powerful agents of change, observing, anticipating, and responding to the health issues of the day, with a voice that resonates across the entire medical system.
How Can this Report be Used to Create Health Policy?
This report invites healthcare stakeholders to recognize the importance of EDs as barometers of overall system health, and emergency physicians as repositories of health system expertise. However, for any system to be functional, there must be an ever-present focus on purpose. We believe the Quintuple Aim [4] is the best framework to guide healthcare policy, and we’ve used it to inform the development of the EM:POWER report and recommendations.
Detailed action plans that cater to population needs will be essential to ensure the report has ongoing value. These are largely the purview of provincial health authorities and Emergency Care Clinical Networks [5] which we recommend be established to lead and coordinate clinical services and HHR planning. The report itself provides the framework and flexibility to allow local autonomy and decision-making; but the federal government holds a key coordinating role to connect provincial/territorial leadership from across Canada to help address common challenges. These include crowding, closures, and Health Human Resources (HHR) as well as to facilitate the establishment of accountability frameworks and disaster preparedness.
It is important for decision-makers to realize that the journey to a more cohesive and functional system will be daunting, take time, and will not conform to political cycles and exigencies. Strategies arising from this report must be based on a clear, depoliticized, long-term vision, with short, medium, and long-term objectives. This avoids the one problem, one solution trap that ultimately fails and reverts to emergency backlogs.
The Practice of Emergency Medicine and CAEP Advocacy
Advocacy can be an important part of an emergency career, giving a sense of agency and connection to the larger problems that underlie our daily work lives. Organized emergency medicine can provide a powerful platform for addressing societal needs that manifest first or frequently in our EDs.
Beyond the current focus on crowding and closures, CAEP has also articulated positions on topics such as violence in the ED, opioid use disorder, gun control, intimate partner violence, homelessness, and care of the elderly. In addition, our organization is currently leading advocacy for national red flag laws to protect those at imminent risk of harm, such as victims of intimate partner violence, those with mental health disorders and the elderly. [8] These topics are linked by way of their prevalence in vulnerable populations or those suffering health inequities. All visit our emergency departments, often feeling they have no other recourse.
During the first year of the pandemic, nimbleness was the order of the day, and a small kitchen cabinet of CAEP executive and public affairs leadership developed 18 position statements and communiques related to COVID-19, along with hosting over 40 media events. [7] This work was essential to preserving and protecting emergency staff, and to ensuring our patients continued to have access to emergency care.
In a post-pandemic world, access block, and the resulting negative impact on patient health and mortality will dominate the discussion for the foreseeable future. [8] While ED crowding has become an international problem, as we emerge from the pandemic this has been particularly chronic and intractable in Canada. The problem is covered extensively elsewhere in this report, but the necessary changes will only come about if we have effective emergency medicine champions to engage with planners and decision- makers, within and beyond medicine.
Training Future Leaders in Public Affairs
As the EM:POWER Task Force formulated this report, we were frequently asked, “Who is this report’s target audience? Those providing care in the ED or those outside it?” While our proximate audience is within healthcare, the ultimate drivers of change are those who consume it, the citizens of Canada, our patients. They will demand system improvement through their publicly- elected officials. The importance of public affairs to emergency care thus becomes self-evident.
Succession planning is important in any political sphere, and this is no different. There are notable emergency physician public affairs thought leaders, who for decades have increased emergency medicine’s profile and advanced its priorities. However, there is little to no formal education in public affairs within EM training programs, even though those in the ED are inextricably linked to, and impacted by, health policy. EM training programs would therefore do well to include such training within a larger Health System Sciences curriculum [9] to nurture the next generation of public affairs leaders.
Recommendations for Emergency Medicine’s Future Role in Health Policy and Public Affairs
- CAEP should actively engage with federal /provincial/territorial ministries, health policy experts and medical organizations to promote the report and its recommendations.
- Provincial ministries of health should fund and enable Emergency Care Clinical Networks (ECCN) and integrate them with the broader Healthcare system governance structure.
- The Provincial/Territorial Council of Deputy Ministers of Health should establish and fund a National Emergency Care Council to provide expert advice to each provincial ECCN; connect/coordinate provincial leadership from across Canada to help address key challenges (e.g., crowding/closures/human health resources); and assist in the development of accountability networks and disaster preparedness.
- CAEP should continue alliances with organizations who share their goals and objectives such as CMA (Canadian Medical Association), NENA (the National Emergency Nurses Association), IFEM (the International Federation for Emergency Medicine), the Society of Rural Physicians of Canada (SRPC), and the Coalition for Gun Control.
- EM:POWER’s framework recommendations should be presented to provincial and regional ECCNs as a basis for system redesign at a more granular level, based on local population health needs and resources.
- EM training programs should include public affairs as part of a Health Systems Science curriculum, to educate residents and nurture the next generation of public affairs leaders.
References
- The Canada Health Act: An Overview [Internet]. [cited 2023 Sep 20]. Available from: https://lop.parl.ca/sites/PublicWebsite/default/en_CA/ResearchPublications/201954E
- Contact AFCNNMCF|. CTV News. 2023 [cited 2023 Sep 20]. Three stabbed teens were driven from a party to a nearby hospital, only to find that the ER was closed. Their story is one of many. Available from: https://www.ctvnews.ca/health/three-stabbed-teens-were-driven-from-a-party-to-a-nearby-hospital-only-to-find-that-the-er-was-closed-their-story-is-one-of-many-1.6545043
- Kelen GD, Wolfe R, D’Onofrio G, Mills AM, Diercks D, Stern SA, et al. Emergency department crowding: the canary in the health care system. NEJM Catalyst Innovations in Care Delivery. 2021;2(5).
- Nundy S, Cooper LA, Mate KS. The Quintuple Aim for Health Care Improvement: A New Imperative to Advance Health Equity. JAMA. 2022 Feb 8;327(6):521–2.
- Abu-Laban RB, Christenson J, Lindstrom RR, Lang E. Emergency care clinical networks. CJEM. 2022;24(6):574–7.
- Position Statements [Internet]. CAEP. [cited 2023 Sep 6]. Available from: https://caep.ca/advocacy/position-statements/
- Breaking News [Internet]. CAEP. [cited 2023 Sep 20]. Available from: https://caep.ca/breaking-news/
- Varner C. Emergency departments are in crisis now and for the foreseeable future. 2023 Jun 19;195(24):E851–2.
- Gonzalo JD, Chang A, Dekhtyar M, Starr SR, Holmboe E, Wolpaw DR. Health Systems Science in Medical Education: Unifying the Components to Catalyze Transformation. Acad Med. 2020 Sep;95(9):1362–72.
Chapter 13: Emergency Medicine in the Era of Climate Change
|
The overarching purpose of this report is to catalyse system redesign to allow for better emergency care in the future. Climate change is the biggest global health threat of the 21st century, [2] and tackling it is our biggest health opportunity. [3] We exist within a global ecosystem in which the health of our patients and our future ability to treat it are inextricably intertwined with the world around us. [1]
Though emergency medicine has traditionally given little thought to our environment beyond illness resulting from extreme heat or cold, our very ability to do our job with the needed resources is now threatened by the potential for supply chain dysfunction, infrastructure challenges, and social disorder attributable to climate change. These challenges coexist with increased patient presentations for physical and mental health compromise related to wildfires, floods, emerging infectious diseases and much more. [4]
This situation is being met by an emergency medicine workforce that is significantly under-educated on climate-related health issues. Curricular surveys show most medical students are still not being taught about climate change or air pollution, [5] and while research has found that most physicians believe climate change is a health threat, they do not feel prepared to manage the situation. [6] Only a minority of those surveyed by our EM:POWER Task Force feel climate change is a very important (11%) or important (22%) issue facing the Canadian healthcare system overall [EM-POWER survey]. This rate of change in our thinking isn’t keeping up with what’s happening on our planet and is unlikely to achieve a viable outcome because just as time is brain, time is planet.
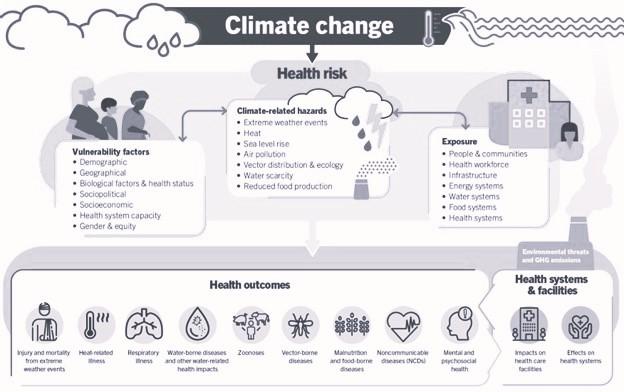
Figure 20. An overview of climate-sensitive health risks, their exposure pathways and vulnerability factors. Climate change impacts health both directly and indirectly, and is strongly mediated by environmental, social and public health determinants. (World Health Organization Report, October 2023)
Emergency medicine must use the breadth and depth of its collective knowledge and skill—in science, education, disease management, bioethics, and advocacy—to address the challenges of this new era of altered planetary physiology: the Anthropocene. [7]
| Physical Health | Zoonoses (infectious diseases spreads from animals to humans)
Heat/Cold Injury Respiratory/Cardiovascular illness Hurricane/Floods/Drowning |
| Mental Health | Geographic displacement and associated mental distress, mood disorders, suicidality.
Weakened social cohesion, violence, aggression |
| Costs* | Increased ED visits
Increased hospital admissions Displaced populations |
| Equity | The greatest impact of climate change is on marginalized populations, such as:
Poor/homeless Visible minorities Workers in hazardous conditions (e.g., construction) Those living in environmentally-fragile areas. Those with pre-existing health conditions Older persons Children Those with disabilities |
| Access | Hospital evacuation
Crowding with decreased access |
| Workforce | Overwork and burnout, leading to attrition.
Increased absenteeism Leaving areas inordinately impacted by climate change |
| Quality | Crowding and boarding with negative care experience
Negative impact on healthcare team well-being Exacerbated health inequity Increased costs Negative impact on population health Supply chain disruption |
Table 6. Impact of climate change on health and health systems [8]
*Findings replicated by the Canadian Climate Institute [9]
Priority Areas for Action and Recommendations
There are four priorities for emergency medicine as we reframe health and healthcare on a planet whose ecological foundations have become unstable:
- Adapt to emerging conditions, now and in the near future.
- Mitigate the trajectory of change.
- Educate ourselves, our patients, and our elected leaders.
- Do our part to make planetary health a societal priority.
Adaptation
Climate emergencies are already increasing in frequency and severity. There must be an understanding within emergency programs of local climate risks, along with adaptation of design and operational plans:
- Emergency physician leaders should be familiar with patient population-health, and ED operational impacts of current climate change events, such as wildfires, prolonged heat events, floods, and population displacement.
- Canada has a National Adaptation Strategy for climate change, [10] which hosts a Disaster Risk Reduction table. Much of this is relevant to emergency physicians and should be integrated into EM training (see Education below). Emergency medicine disaster experts should be integral parts of this conversation and sit at the table.
Mitigation
While measures to combat climate change are the foundation of our response to this crisis, it remains true that, whatever our response, some of the impacts of climate change will remain with us for years to come. Because of this, mitigation of potential immediate-term risks is critical:
- ED directors must be aware of the temperature and precipitation projections for their region, plan for the consequent operational impacts, and work with climate-savvy architects and engineers to design infrastructure for a changing environment, and
- Emergency medicine leaders must collaborate with governments and other healthcare stakeholders to ensure the necessary supply of pharmaceuticals and other products and mitigate their impact on the environment.
Education
Teaching of climate-related emergencies within a broader understanding of the Anthropocene should be part of residency training and continuing professional development. There is evidence that the general population underestimates the immediate risks of climate change on health—such as mental health, infectious diseases, and heat-related illnesses. [11] Physicians therefore have roles as both learners and public educators in climate change:
- Because emergency physicians are familiar with treating patients impacted by extreme heat, wildfires, and floods, they should increase their role in public education related to climate change and climate emergencies, and
- CAEP should harness its internal expertise in education, research, and public affairs—along with allies from other disciplines—to help illustrate and mitigate the health impacts of climate change.
Prioritization: Make Health and Wellbeing an Overarching Goal
It will be impossible to create a highly functional health ecosystem in any individual country within a destabilized global ecosystem. Currently, no country meets its population’s basic needs while keeping resource use at a sustainable level. [12] And modelling suggests that it will be difficult to continue to increase growth in GDP while decreasing its impact on the planet. [13] This puts us at risk of crossing global tipping points that could lead to runaway warming and vast destabilization, the so-called hothouse earth. [14] An urgent dialogue is necessary to reframe our social priorities, and as stewards of the health system, physicians must necessarily become stewards of the planet as well.
Conclusion
The foundations of human health and health systems are being destabilized by climate change. All health professions require a reframing of their priorities and redesign of their systems to include an evidence-based, values-driven response to the ecological emergency facing us. This includes expanded education and professional development, engagement in national and provincial adaptation strategies, and leadership in the public domain. It’s a daunting challenge, but if there’s any specialty with the skill and character to adapt to rapidly-changing conditions, it’s emergency medicine. A broad understanding of the urgency and complexity of the emergency before us is lacking, but there is no shortage of information—and no time to waste.
Additional Reading
- The theme of direct health impacts caused by future weather and climate is frequently noted in the Canada’s Changing Climate series subject area reports, which are essential reading for physicians.
- The Climate Atlas of Canada has a very accessible library of short articles, and the health section has some directly relevant topics.
- From the World Health Organization, the direct impact of climate change on health.
References
- Chochinov A, Petrie DA, Kollek D, Innes G. EM:POWER: if not us, who? If not now, when? CJEM. 2023 Jan;25(1):11–3.
- WHO issues urgent call for global climate action to create resilient and sustainable health systems [Internet]. [cited 2023 Jun 29]. Available from: https://www.who.int/news/item/24-05-2023-wha76-strategic-roundtable-on-health-and-climate
- Watts N, Adger WN, Agnolucci P, Blackstock J, Byass P, Cai W, et al. Health and climate change: policy responses to protect public health. Lancet Lond Engl. 2015 Nov 7;386(10006):1861–914.
- Romanello M, Di Napoli C, Drummond P, Green C, Kennard H, Lampard P, et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet Lond Engl. 2022 Nov 5;400(10363):1619–54.
- Omrani OE, Dafallah A, Paniello Castillo B, Amaro BQRC, Taneja S, Amzil M, et al. Envisioning planetary health in every medical curriculum: An international medical student organization’s perspective. Med Teach. 2020 Oct;42(10):1107–11.
- Kotcher J, Maibach E, Miller J, Campbell E, Alqodmani L, Maiero M, et al. Views of health professionals on climate change and health: a multinational survey study. Lancet Planet Health. 2021 May;5(5):e316–23.
- Redvers N, Faerron Guzmán CA, Parkes MW. Towards an educational praxis for planetary health: a call for transformative, inclusive, and integrative approaches for learning and relearning in the Anthropocene. Lancet Planet Health. 2023 Jan;7(1):e77–85.
- The Impact of Climate Change on Our Health and Health Systems [Internet]. 2022 [cited 2023 Jun 29]. Available from: https://www.commonwealthfund.org/publications/explainer/2022/may/impact-climate-change-our-health-and-health-systems
- The health costs of climate change [Internet]. Canadian Climate Institute. [cited 2023 Jun 29]. Available from: https://climateinstitute.ca/reports/the-health-costs-of-climate-change/
- Canada S. Canada’s National Adaptation Strategy: Building Resilient Communities and a Strong Economy [Internet]. 2021 [cited 2023 Jun 29]. Available from: https://www.canada.ca/en/services/environment/weather/climatechange/climate-plan/national-adaptation-strategy.html
- Casson N, Cameron L, Mauro I, Friesen-Hughes K, Rocque R. Perceptions of the health impacts of climate change among Canadians. BMC Public Health. 2023 Jan 31;23(1):212.
- Fanning AL, O’Neill DW, Hickel J, Roux N. The social shortfall and ecological overshoot of nations. Nat Sustain. 2022 Jan;5(1):26–36.
- O’Neill D. Beyond green growth. Nat Sustain. 2020 Mar 1;3:1–2.
- Steffen W, Rockström J, Richardson K, Lenton TM, Folke C, Liverman D, et al. Trajectories of the Earth System in the Anthropocene. Proc Natl Acad Sci. 2018 Aug 14;115(33):8252–9.
Chapter 14: Building on Values: Justice, Equity, Diversity, and Inclusion (JEDI)
Health equity is defined as “the state in which everyone has the opportunity to attain their full health potential, and no one is disadvantaged from achieving this potential because of social position or other socially determined circumstances.” [4] The causes of health inequity do not begin or end with the health system, but with the social determinants of health that impede some groups from having access to the resources and opportunities others enjoy.
As respected members of society, physicians can and should be powerful advocates for social justice to ensure healthy living conditions for all. Most urgently, however, it is incumbent on us to tackle the systemic discrimination that persists within our own health system. This chapter will outline some of the ways we can do so, with a focus on ED staffing, leadership, and care of marginalized populations. It is important to note that the implications of JEDI go far beyond this brief overview; JEDI should inform all aspects of emergency care planning and be considered in relation to all sections of this report.
Many diverse and marginalized populations do not feel safe accessing care in the ED, often sensing that they are not heard and their needs are not addressed. [5,6,7,8,9] The scourge of anti-Indigenous racism has contributed to tragic deaths like those of Brian Sinclair [10] and Joyce Echaquan. [11] Healthcare is also plagued by additional types of racism, as well as ageism, ableism, sexism, homophobia, transphobia, and other forms of discrimination. An important part of the solution is to ensure the diversity of Canada’s population is reflected in its healthcare system. [12, 13] Representation matters; it has profound impacts on how people view and use the system, trust providers, and adhere to healthcare recommendations that affect patient outcomes. [14,15,16] Despite small advances in this area, significant disparities continue to exist among physicians with respect to representation, level of advancement, and salaries by gender, age, and race/ethnicity. [17,18,19] Research demonstrates increasing harassment, sexual assault, hiring bias and pay inequity among women and racialized minorities, even when accounting for education, academic rank, geographic training, clinical hours worked, years of experience, and administrative roles. [17,12,20,21] The effects are further increased if someone identifies as being part of more than one equity-deserving group. [12] Just a few years ago, an Ontario ED was discovered to not have hired a female physician for 16 years, despite women making up over 40% of ED residents. [22] Hospitals and healthcare systems must ensure that they employ diverse hiring panels, mandate training to mitigate bias and regularly review staff makeup to evaluate whether it represents the population it serves. [23]
The lack of diversity is even greater within leadership positions, where racialized individuals are considerably lacking. Without diversity, teams miss key perspectives to guide decision-making and engender mistrust in underrepresented communities. Diverse leadership may be more likely to promote culturally sensitive care and foster a culture of anti-racism among staff and is thought to also improve patient experiences and outcomes. [12]
In addition to diversifying leadership and workforce, efforts should also be made to educate healthcare staff on the impacts of discrimination in medicine and incorporate JEDI into medical education (24). It’s essential that all healthcare staff are trained to provide culturally-safe care to the diverse populations we serve. [25,26] A diverse workforce with proper training in JEDI has the potential to decrease treatment disparity, increase cultural sensitivity, and inform policymaking to facilitate change. [27]
Several other JEDI-promoting initiatives should be adopted as we move forward:
Enhance Inclusivity
Some easy-to-implement changes to enhance inclusivity within the ED include posting non-discrimination policies, using visuals that promote diversity, offering population-specific resources, and creating “all-gender” bathrooms. [28]
Collect More Data
It is essential to properly capture ED patients’ gender identity. [26] In order to better understand the community that the ED serves, efforts should be made to collect expanded sociodemographic data, particularly race and ethnicity. Barriers to care, such as transportation, food insecurity and housing, also need to be gathered. [26,29,30,31,16] Data must be leveraged to ensure we understand our patients’ diversity, address the right problems, and evaluate our change processes.
Equitable Technology
It’s important to ensure that the adoption of new digital technologies—especially those delivered privately—doesn’t increase health disparities by providing care only to those who can afford the technology or have the cultural comfort and health literacy to use it. [32,33,34,35,36] Care should also be taken when implementing AI-based technology, to ensure biases are not further amplified.
Diverse Voices of Patients
As we look ahead, the patient voice, including diverse perspectives, must inform ED co-design and policy development, fulfilling the dictum nothing about us without us. [37,29]
Impact of Stress on Provider Bias
Finally, we note the synergy between the promotion of JEDI and the overall aims of this report. As the safety net for Canadians, the ED is the primary locus of care many patients whose health is affected by adverse social and economic conditions. Lacking access to care through other means, they are disproportionately impacted as the quality of ED care drops. [38] The stress of working in an understaffed, overstretched ED can impair a provider’s decision-making, increasing the chance that racial and other biases will pollute clinical judgement that further exacerbates differences in care between populations. All measures required to create a functional system of emergency care, as discussed in other chapters, are also crucial to the pursuit of JEDI.
In addition to the recommendations below, we encourage you to read the excellent submission by the CAEP Health Equity Subcommittee (Appendix 2).
Recommendations for Building on Values: Justice, Equity, Diversity, and Inclusion
(JEDI) in Emergency Medicine
- Emergency care programs (ECPs) should promote diversity within leadership and among healthcare staff, to better understand and care for the communities they serve.
- ECPs should foster patient and community engagement from marginalized groups in clinical service planning and delivery.
- All ECP staff must undergo formal training to better understand the different cultures and populations they serve.
- ECPs should expand the collection and utilization of sociodemographic data to better evaluate and address JEDI within their programs. There should be public reporting of key operational outcomes that impact marginalized and oppressed populations.
- Academic departments of emergency medicine should contribute to the understanding and amelioration of inequities in emergency care delivery by supporting JEDI-focused research and multidisciplinary special interest groups (SIGs).
- JEDI must be a paramount consideration as digital health is incorporated into Canada’s healthcare system.
References
- Government of Canada PS and PC. Building on values: the future of health care in Canada: final report / Roy J. Romanow, Commissioner. : CP32-85/2002E-IN – Government of Canada Publications – Canada.ca [Internet]. 2002 [cited 2023 Jun 29]. Available from: https://publications.gc.ca/site/eng/237274/publication.html
- Just society. In: Wikipedia [Internet]. 2023 [cited 2023 Jun 29]. Available from: https://en.wikipedia.org/w/index.php?title=Just_society&oldid=1149571975
- The Canadian Charter of Rights and Freedoms [Internet]. [cited 2023 Jun 29]. Available from: https://www.justice.gc.ca/eng/csj-sjc/rfc-dlc/ccrf-ccdl/
- Ramirez LKB, Baker EA, Metzler M. Promoting Health Equity: A Resource to Help Communities Address Social Determinants of Health: (540452013-001) [Internet]. 2008 [cited 2023 Jun 29]. Available from: http://doi.apa.org/get-pe-doi.cfm?doi=10.1037/e540452013-001
- Understanding and Ameliorating Medical Mistrust Among Black Americans [Internet]. 2021 [cited 2023 Jun 29]. Available from: https://www.commonwealthfund.org/publications/newsletter-article/2021/jan/medical-mistrust-among-black-americans
- Canada H. Certain Circumstances Issues in Equity and Responsiveness in Access to Health Care in Canada [Internet]. 2003 [cited 2023 Jun 29]. Available from: https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-accessibility/certain-circumstances-issues-equity-responsiveness.html
- CBC · DBG·. CBC. 2015 [cited 2023 Jun 29]. Ageism still rampant in health care | CBC Radio. Available from: https://www.cbc.ca/radio/whitecoat/blog/ageism-still-rampant-in-health-care-1.3139864
- Canada PHA of. Infographic: Inequalities in mental illness hospitalization in Canada [Internet]. 2019 [cited 2023 Jun 29]. Available from: https://www.canada.ca/en/public-health/services/publications/science-research-data/inequalities-mental-illness-hospitalization-infographic.html
- Kim PJ. Social Determinants of Health Inequities in Indigenous Canadians Through a Life Course Approach to Colonialism and the Residential School System. Health Equity. 2019 Jul 25;3(1):378–81.
- Ignored to death: Brian Sinclair’s death caused by racism, inquest inadequate, group says | CBC News [Internet]. [cited 2023 Aug 14]. Available from: https://www.cbc.ca/news/canada/manitoba/winnipeg-brian-sinclair-report-1.4295996
- News · AN· C. CBC. 2021 [cited 2023 Aug 14]. Racism, prejudice contributed to Joyce Echaquan’s death in hospital, Quebec coroner’s inquiry concludes | CBC News. Available from: https://www.cbc.ca/news/canada/montreal/joyce-echaquan-systemic-racism-quebec-government-1.6196038
- Sergeant A, Saha S, Lalwani A, Sergeant A, McNair A, Larrazabal E, et al. Diversity among health care leaders in Canada: a cross-sectional study of perceived gender and race. CMAJ Can Med Assoc J J Assoc Medicale Can. 2022 Mar 14;194(10):E371–7.
- Canadian Medical Association [Internet]. [cited 2023 Jun 29]. Addressing gender equity and diversity in Canada’s medical profession: A review. Available from: https://www.cma.ca/physician-wellness-hub/resources/equity-and-diversity-medicine/addressing-gender-equity-and
- Togioka BM, Duvivier D, Young E. Diversity and Discrimination in Healthcare. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 Jun 29]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK568721/
- Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Aff Proj Hope. 2002;21(5):90–102.
- Kalich A, Heinemann L, Ghahari S. A Scoping Review of Immigrant Experience of Health Care Access Barriers in Canada. J Immigr Minor Health. 2016 Jun;18(3):697–709.
- Madsen TE, Linden JA, Rounds K, Hsieh YH, Lopez BL, Boatright D, et al. Current Status of Gender and Racial/Ethnic Disparities Among Academic Emergency Medicine Physicians. Acad Emerg Med Off J Soc Acad Emerg Med. 2017 Oct;24(10):1182–92.
- Sheppard G, Pham C, Nowacki A, Bischoff T, Snider C. Towards gender equity in emergency medicine: a position statement from the CAEP Women in Emergency Medicine committee. CJEM. 2021 Jul;23(4):455–9.
- Canada E and SD. Discussion guide on ageism in Canada [Internet]. 2022 [cited 2023 Jun 29]. Available from: https://www.canada.ca/en/employment-social-development/corporate/seniors/forum/consultation-ageism/discussion-guide.html
- What’s Holding Women in Medicine Back from Leadership [Internet]. [cited 2023 Jun 29]. Available from: https://hbr.org/2018/06/whats-holding-women-in-medicine-back-from-leadership#
- Marco CA, Geiderman JM, Schears RM, Derse AR. Emergency Medicine in the #MeToo Era. Acad Emerg Med Off J Soc Acad Emerg Med. 2019 Nov;26(11):1245–54.
- Ontario emergency room chief who hired no women for 16 years resigns amid discrimination probe – The Globe and Mail [Internet]. [cited 2023 Jun 29]. Available from: https://www.theglobeandmail.com/canada/investigations/article-ontario-emergency-room-chief-who-hired-no-women-for-16-years-resigns/
- Kuhn GJ, Abbuhl SB, Clem KJ, Society for Academic Emergency Medicine (SAEM) Taskforce for Women in Academic Emergency Medicine. Recommendations from the Society for Academic Emergency Medicine (SAEM) Taskforce on women in academic emergency medicine. Acad Emerg Med Off J Soc Acad Emerg Med. 2008 Aug;15(8):762–7.
- Barnabe C, Osei-Tutu K, Maniate JM, Razack S, Wong BM, Thoma B, et al. Equity, diversity, inclusion, and social justice in CanMEDS 2025. Can Med Educ J. 2023 Mar 21;14(1):27–32.
- Williams DR, Rucker TD. Understanding and Addressing Racial Disparities in Health Care. Health Care Financ Rev. 2000;21(4):75–90.
- Leeies M, Grunau B, Askin N, Fesehaye L, Kornelsen J, McColl T, et al. Equity‐relevant sociodemographic variable collection in emergency medicine: A systematic review, qualitative evidence synthesis, and recommendations for practice. Acad Emerg Med. 2022;
- Nair L, Adetayo OA. Cultural Competence and Ethnic Diversity in Healthcare. Plast Reconstr Surg Glob Open. 2019 May 16;7(5):e2219.
- pdf [Internet]. [cited 2023 Jun 29]. Available from: https://rnao.ca/sites/rnao-ca/files/bpg/2SLGBTQI_BPG_June_2021.pdf
- Pinto AD. Can a Focus on Equity, Diversity and Inclusion Transform Health Services Research. Heal Pap. 2022 Apr;20(3):53–60.
- Deb S, Sud M, Wijeysundera HC. If You Can’t Measure It, You Can’t Improve It: Data Collection and Standards in the Evaluation of Racial and Ethnic Disparities in Cardiovascular Disease. Can J Cardiol. 2023 May 11;S0828-282X(23)00386-0.
- Fraze T, Lewis VA, Rodriguez HP, Fisher ES. Housing, Transportation, And Food: How ACOs Seek to Improve Population Health By Addressing Nonmedical Needs Of Patients. Health Aff Proj Hope. 2016 Nov 1;35(11):2109–15.
- News · DBG· C. CBC. 2020 [cited 2023 Jun 29]. The health cost of being poor | CBC Radio. Available from: https://www.cbc.ca/radio/whitecoat/the-health-cost-of-being-poor-1.5449683
- Affleck E. Inequity in Digital Health Planning in Canada. Healthc Pap. 2022 Apr;20(4):37–43.
- Koehle H, Kronk C, Lee YJ. Digital Health Equity: Addressing Power, Usability, and Trust to Strengthen Health Systems. Yearb Med Inform. 2022 Dec 4;31(1):20–32.
- Miller A, News · BS· C. CBC. 2022 [cited 2023 Jun 29]. Would more privatization in Canadian health care solve the current crisis? | CBC News. Available from: https://www.cbc.ca/news/health/canada-healthcare-privatization-debate-second-opinion-1.6554073
- Challenges and opportunities for primary care and health equity in the age of technology – Healthy Debate [Internet]. [cited 2023 Jun 29]. Available from: https://healthydebate.ca/2023/05/topic/challenges-opportunities-primary-care-technology/
- Lee TH, McGlynn EA, Safran DG. A Framework for Increasing Trust Between Patients and the Organizations That Care for Them. JAMA. 2019 Feb 12;321(6):539–40.
- Harrell IB. Emergency Departments and Care for Marginalized Populations. [cited 2023 Jun 29]; Available from: https://digitalcommons.odu.edu/humanities_etds/17/
Chapter 15: Lessons from Other Healthcare Systems
This chapter illustratively compares health policy approaches from several OECD countries and identifies potential best practices for Canada, covering the areas of workforce planning, system capacity, long-term care and private vs. public care. To provide inside as well as outside perspectives, we focus on countries in which at least one contributing author has clinical experience: Australia, the UK, and (in the long-term care domain) Sweden. Both Australia and the UK reliably score in the top four of the Commonwealth Fund’s 11-country comparisons, with the UK occupying the top spot for years, until funding cuts began to erode access and equity. [5] Sweden tends to be in a mid-range standing overall, but along with other Scandinavian countries is considered an exemplar in aged care.
Last year, the Canadian Medical Association (CMA) [1] and health policy experts [2,3] outlined healthcare concerns that require bold government action. To achieve our goals, it is essential to be a Learning Health System, [4] open to lessons from the experience of our peers as well as our own.
Workforce Planning
|
CANADA It’s 2am, two hours past end-of-shift. I’ve just seen a patient whose appendix ruptured after 9 hours in our waiting room. An irate woman approaches me. She’s heard there is single physician coverage overnight, and her husband has already waited six hours. I explain that our funding only allows for one night physician, but ask about her husband. He’s had 3 months of abdominal pain, weight loss and cannot get a family. physician since his doctor retired 2 years ago. Six weeks ago, a clinic doctor ordered an ultrasound. The doctor called today, reported that the scan showed an abdominal mass, and told him to go immediately to the ED for further investigation. I order a CT scan and ask the nightshift emergency physician to see him. AUSTRALIA I begin winding down at 9:30pm from a 3pm-11pm shift, but am on call until 8:30 the next morning. The senior registrar (a recent overseas hire) has arrived with an intern, a junior doctor, and a junior registrar for the night shift. There are 25 patients waiting to be seen, so I continue working until 4am. Earlier that day, a patient with appendicitis was referred in. He arrived with his GP’s notes and a confirmatory CT report. The physician at triage contacted the on-call surgical registrar, and the patient was sent to the surgical assessment unit within the hour. Given increased patient demand, the hospital has created a second physician-triage role for the ambulance bay. There is an oncology hospital connected to our hospital, so I never see patients with undifferentiated masses in the ED. UNITED KINGDOM It’s midnight. I’m covering the night shift for a missing senior trainee. The department is critically overcrowded, with 6 patients blocked in ambulances, 8 children waiting, and over 30 patients in the ambulatory area. I have a junior doctor, three less experienced doctors in training, and one advanced clinical practitioner with me. My colleague who started at 17:00 is tired and hoped to leave at midnight, but has agreed to stay until 02:00. We deploy two clinicians to the paediatric area and send the rest to ambulatory, leaving a skeleton team in the “majors” area. I apologize to patients in the ambulatory area, telling them they will be waiting many hours, perhaps all night, and if they need admitting they will likely spend the night on chairs since we have no more trolleys. I’ve made this announcement so often it’s second nature. |
Workforce Overview
In 2021, Australia, the UK and Canada had 3.9, 3.1 and 2.8 physicians per 1000 population respectively. [6] Australia also has more nurses (12.8 nurses/1000) than Canada (10.1) and the UK (8.7) (7). Many Canadian physicians are independent contractors, invoicing their provincial healthcare system on a fee-for-service basis. [8] In recent decades, many physician groups have negotiated alternate funding arrangements (AFA) with their provincial health ministries.
AFA contracts pay a defined income for specified work expectations; however, typically they preserve the physician’s independent practitioner status and do not provide pensions, sick time, vacation, health, or dental benefits. [9] Unlike their Canadian counterparts, Australian and UK hospital physicians are salaried employees. Compensation packages for physicians in Australia include retirement funds, prorated sick, annual, and 10-year service leave.
In Canada, physicians-in-training are employed by the university and require supervision until they’re eligible for licensure after a 2- to 7-year residency/fellowship. In contrast, Australian and UK physicians are licensed after their first postgraduate year (Foundation Year 1) and can practice independently. Australia and the UK have a higher physician workforce than Canada because of their large unsupervised physician-in-training staff who work at disadvantaged hours (up to 12 years in some cases) for less pay than consultants.
Canada
Canadian provinces pursue workforce strategies without interprovincial integration. Overall, personnel planning is fragmented, with insufficient planners using unstandardized data. As an example, Ontario’s Ministry of Health has a Workforce Planning Branch, [10] but its three databases are disconnected, not linked to medical training data, and do not provide trends or supply-demand analyses. [11,12,13] In addition, past provincial workforce planning models have not differentiated between certified emergency physicians (FRCP and CCFP-EM) and family physicians who work ED shifts as part of comprehensive rural family practice. There is also insufficient data on the number of ED hours/year, and trends worked by family physicians. Consequently, workforce planners would be unable to estimate how many new FRCP and CCFP-EM training positions are required to fill the current and growing gap in ED coverage (see Chapter 2).
In Canada, private recruiters pursue overseas healthcare staff; however, these individuals often learn post-migration that they lack the qualifications to work here. [14] Some provinces, including New Brunswick and Alberta, [15,16] use financial incentives to “poach” healthcare workers across provincial borders. Canada’s licensure is provincial, and healthcare workers can only work where they are specifically licensed. As of 2023, Ontario has now recognized the credentials of workers registered in other provinces and territories. [17] This move towards national registration is positive but will likely facilitate further poaching from other provinces. [18]
In 2016, the Collaborate Working Group on the Future of Emergency Medicine in Canada, created by CAEP, the Royal College of Physicians and Surgeons and the College of Family Physicians projected a national shortfall of 1,518 emergency physicians by 2025. [19] However, the recommendations of the report were not implemented by governments, resulting in no meaningful changes to workforce planning.
Australia
Research has suggested that Australia’s approach to workforce planning and accreditation is superior to Canada’s because of its strong federal involvement. [20,21] The Australian federal government coordinates workforce planning, training, interdisciplinary engagement, integration, adaptation, and strategic planning across all health disciplines. It uses comprehensive supply and demand data that describes training, migration, workforce aging, service use, and population demographics.
Workforce models are analyzed iteratively, using varying assumptions, as well as estimates derived from stakeholder engagement. Retention scenarios are also inputted into workforce models. [22] The Australian government has developed many proactive 10-year strategic plans. [23,24,25] These address regional shortages by augmenting the rural and remote workforce, using immigration policy and controlling Medicare provider numbers to adjust the number of overseas-trained physicians, and by funding medical students. [26,27] State and territorial governments staff public hospitals, provide training placements, and identify workforce shortfalls.
Australia has a unified national registration that ensures standardization of all 15 regulated health professions and allows practice across state and territorial borders. [28] With global physician and nurse shortages, international recruitment is controversial; [29] an exodus of UK physicians to Australia and New Zealand has exacerbated UK shortages, and Australia has been criticized for poaching. [30,31] The Australian Nursing and Midwifery Federation has recommended an increase in domestic training and declared that aggressive international recruitment is unethical. [32] To promote worker retention and limit interstate poaching, the New South Wales parliament abolished wage caps for junior doctors, paramedics, nurses, and other healthcare staff. [33]
Post-pandemic, unanticipated senior staff departures created ED physician shortfalls, especially in rural hospitals. In response, the Australian College of Emergency Medicine (ACEM) developed guidelines for retaining senior emergency physicians. [34] Meanwhile, locums or junior on-call physicians cover nightshifts, [35] and senior ED physicians use virtual care links for review and supervision. [36] Many small rural hospitals that were previously managed by general practitioners have, in effect, lost their emergency departments, [37] and instead, nurses provide urgent care with virtual support. In some regions, the virtual ED physician is the only doctor available.
Australian virtual care also supports ambulance services, aged care, and primary healthcare networks; patient-initiated virtual consults with emergency physicians are available but require co-payment. This shift to virtual care has raised concerns about service duplication, lack of care coordination, care delays and questionable cost-effectiveness. [38]
United Kingdom
In England, workforce planning is national; however, it has been inconsistent, based on payroll data that does not adjust for part-time workers, and misclassifies providers by their contract status, rather than their function. The NHS is awaiting publication of an updated workforce plan.
England, as of June 2022, has a staffing crisis with 133,000 vacancies, of which 9,000 were medical. The Royal College of Emergency Medicine (RCEM) estimates the UK will need 6,300 whole time equivalent (WTE) EM consultants by 2038 but will fall 600 short. This does not account for changes that will extend consultant working hours overnight in major centres. In addition, many junior doctors are leaving to work overseas, and senior doctors are retiring early. Trends within the nursing workforce are poorly understood, but sustainability is a major concern. The NHS is adding non-physician roles for advanced clinical practitioners and physician associates, but their impact is uncertain, and many are leaving emergency medicine for primary care.
Learnings
Canada can learn from Australia’s federal involvement and nationalized approach to the integration of data, regulation of healthcare disciplines, workforce supply-demand calculations, and 10-year strategic plans. It aligns with the Savage Model [39] discussed in Section Two (Optimize Access Points), Chapter Six of this report. The Task Force endorses CMA recommendations that Canada develop a national workforce strategy and eliminate interprovincial mobility barriers. This should involve national, or at minimum, provincial workforce planning, using a standardized approach to data, measurement, and prediction as well as considering the effects of evolving provider work patterns and population aging. [40]
We recommend Canada expand physician capacity by increasing from the current 2.8 doctors per 1000 population to the OECD average of 3.6, [6] with distribution matching population need by type and geography. This can be accomplished partially through a judicious immigration policy, keeping in mind ethical concerns around poaching from countries with more severe provider shortfalls. Canada’s physician workforce should grow primarily by expanding medical school enrollment, and through providing opportunity for many more Canadians.
To benefit underserved regions, Canada should introduce incentives to attract physicians to high-need specialties, such as emergency medicine. The health workforce capacity could also be enhanced by promoting the concept of working to full scope. This would mean greater (and graded) responsibility for residents and trainees. To complement the physician workforce, roles for nurses, pharmacists, social workers, nurse practitioners and even volunteers could be expanded as members of the emergency team. Because of Canada’s licensing and training requirements, we are unlikely to move to the Australian model of licensed independent junior doctors; we therefore strongly advocate for increased training positions and national portability for emergency physicians.
System Factors: Hospital Capacity and Time Targets
|
CANADA As my shift begins, there are 56 admitted patients waiting in the ED for an inpatient bed, several for over 48 hrs. Six are critically ill, waiting for ICU. In the hallway, I see a patient with a new pancreatic mass, whom I referred to General Internal Medicine two days ago. The patient is being discharged today with their entire 51-hr hospitalization spent in the ED. This unfortunate situation reminds me of a recent study comparing an Australian and Canadian ED. Between 2012 and 2016, as the Australian hospital’s occupancy increased from 87.6% to 89.7%, the hospital increased its hospital beds from 714 to 930 and short-stay beds from 8 to 14. In contrast, when the Canadian hospital’s occupancy increased from 97.6% to 99.6%, the hospital decreased its acute bed count from 343 to 313. It does not have a short stay unit. [41] AUSTRALIA Four admitted patients are waiting in the ED, but none is critical. During a typical shift, we admit 15 patients who move to a ward within 16 hrs. Today, only 10% of admissions achieved the 4-hour NEAT (56) target. I’ve assessed a patient with right upper quadrant pain whose bloodwork is pending. She is almost at 4 hrs, and her presentation seems like biliary colic, so I enter a bed request, consult General Surgery, and transfer her to the surgical assessment unit to ensure NEAT isn’t breached. I send an older patient post-fall to our 30-bed short stay unit (SSU) where patients can stay for 24 hours. I hand the patient over to an intern I haven’t met before, but an SSU consultant will take over. My colleague informs me that her ED has admissions boarding for over 20 hrs. They plan to expand their short stay unit, but there will be delays due to staff shortages. UNITED KINGDOM I come on shift at 1700. Our resuscitation and major areas cubicles are all full, and patients are lining the corridors. I recognize several patients still here from yesterday. Many are older persons, some confused. Our “HALO” area, a decommissioned clinical decision unit staffed by paramedics and designed to facilitate ambulance offloads, is also full. If I need a resuscitation cubicle, I will have to rapidly decant a patient into a corridor space. There are 15 patients in ambulances waiting to be offloaded, so I send nurses and doctors out to care for them. The longest offload delay is over 6 hours, and the longest wait in the emergency department is 36 hours. My first job is to apologize to the family of a patient who came in yesterday and died in a side room because there was no inpatient bed for her. The family is understanding because they have seen the conditions in our ED, but for the patient it’s too late, and the nursing staff are upset she could not be cared for in a more suitable area. |
System Overview
Canadian healthcare governance is provincial; consequently, Canada has 14 separate healthcare systems, one for each province and territory, plus a federal system for First Nations people living on reserves, members of the armed forces and other specific populations. Provinces and territories currently provide 78% of health funding, while the federal government contributes 22%. [42]
Australia’s healthcare system is also federated with a similar division of federal and provincial powers; however, unlike Canada, there has been a trend towards more centralization with greater federal involvement. [20] Australia’s public hospitals are co-funded by federal, state and territory governments. The federal share increased from 40% to 50% by January 2020 because of the COVID-19 pandemic. [43] Funding is aggregated in the National Health Funding Pool, then distributed to Local Hospital Networks [44] that are third parties for local hospital networks, state health departments and providers. [43]
The UK has a National Health Service (NHS), nationally funded but administered by separate arm’s-length bodies for England, Scotland, Wales, and Northern Ireland.
While all three nations’ systems are somewhat devolved, Canada’s is the most decentralized, [2] and arguably the least actively managed.
In 2019, Canada had 2.5 hospital beds per 1,000 population, compared to Australia’s 3.8, and the OECD average of 4.4. [48] According to the World Bank, Australia’s 2019 health expenditure per capita of $5,427USD was greater than Canada’s $5,048; however, Canada’s expenditure represented a higher percentage of GDP than Australia’s (11.0% vs. 10.2%). [46] The UK, at the end of a decade of austerity measures, stood at $4,265 spending per capita (9.9% of GDP) [46] and 2.4 hospital beds per population. [45]
Canada
Most Canadian hospitals rely on global budgets negotiated with their health ministries, but Ontario, Quebec, and BC have shifted toward activity-based funding, where financing is dependent on the care and services provided. [47,48,49] The Ontario Ministry of Health (MOH) distributes funding largely through global budgets, Quality Based Procedures (QBP) and Health-based Allocation Models (HBAM). [48,50,51] HBAM allocates funding based on expected expenses that takes annual case volume with clinical, social, and demographic weight factors into consideration. It provides 38% of hospital funding, but there is a fixed total funding envelope, so if all the expected expenses at a hospital increases, the individual funding may not. [50] For QBP, which accounts for up to 30% of funding, a hospital must achieve specified quality outcomes for procedures, such as hip replacements.
Many Canadian jurisdictions have, at various times, set targets for ED wait times or length of stay. Generally, however, such targets have been too weakly enforced to constitute a meaningful policy lever. [52] Where the (non) achievement of targets has been attached to consequences, these tend to be carrots rather than sticks. Hospitals in Ontario, and formerly BC, did receive pay-for-performance funds for achieving time targets. [48,53,54] Such funds are often reinvested in flow-improvement interventions such as observation units, [9] a strategy associated with modest benefits in some jurisdictions, though not in others. [53]
Australia
Australia’s public hospitals operate mainly through activity-based funding, where the number, mix and complexity of patients are considered, [29,55] but some rural and regional hospitals receive block or global funding.
In 2012, evidence linking ED crowding with mortality prompted Australia to adopt the National Emergency Access Target (NEAT), under which 90% of all ED patients should leave the department within 4 hours. [56]
However, NEAT’s outcomes were mixed and ultimately did not reach the four-hour target.
The substantial investments to achieve NEAT included [57]:
- Staffing augmentation, such as RN flow coordinators
- ED physician in charge
- Expanded working hours
- More allied healthcare workers
- New care models, and
- New hospital policies.
The new care models included short-stay units, team-based care, fast track, senior physician at triage, admit streaming, medical and surgical assessment units, and discharge transit lounges. And the new hospital policies introduced single call admission, over-census escalation, direct admission, and bed allocation,
The initiative reduced 30-day mortality in Western Australia, but not in other states, [58] and most hospitals could not achieve NEAT, especially for admissions. [56] Unintended consequences became evident. As patients approached the 4-hour mark, staff became stressed to abruptly prioritize them, resulting in data manipulation, gaming, decision-making and compromised care quality. [56,57,59] NEAT also compromised communication, morale, teamwork, and education, negatively impacting organizational resilience, sustainability, and clinical outcomes. [60])
Despite NEAT, access block has persisted and worsened since COVID-19. A recent review by ACEM (the Australian College of Emergency Medicine) [61] recommended:
- Reducing bed occupancy from 95% to 85% by increasing inpatient capacity
- Establishing adequately resourced, meaningfully used short-stay units (not to serve as holding wards)
- Expediting ED to inpatient transitions, and
- Balancing time targets with patient safety metrics.
The New South Wales parliament [33] adopted ACEM’s 85% occupancy recommendation, abolished healthcare wage caps to ensure retention, and implemented several service increases and process improvements. There was no time target recommendation because of concern about its punitive consequences. [33]
United Kingdom
Between 2003 and 2008, the UK shifted from global budgets to activity-based funding for hospitals. During this period, patient volumes increased, and length of stay decreased; however, as other major interventions were occurring simultaneously, it’s difficult to assess how much the shift in funding contributed to these outcomes. [62]
In 2004, the government implemented a new standard, which required 95% of ED patients to be admitted, transferred, or discharged within 4 hours. Early top-down efforts to achieve this were often obscured by data manipulation and failed. [63] Later efforts focused on demand management, hospital process improvement, and changes to emergency care. These did dramatically reduce the proportion of ‘long waiters’, although the change was achieved in part by hastily admitting patients nearing the 4-hour mark. The average ED length of stay, however, did not decrease. [64] The 4-hour standard was last met in 2011, and system performance has since declined, despite many initiatives designed to meet this constitutional standard. Ambulance response times, offload delays, [65] and numbers of patients waiting more than 12 hours in emergency departments have all increased substantially. [64] Estimates by the Royal College of Emergency Medicine (RCEM) suggest that up to 500 UK patients die every week because of emergency care delays. [66]
An important part of the picture is that hospital capacity has decreased; there are now about half as many hospital beds in the UK as there were 30 years ago. [67] The UK’s beds-per-population ratio is now lower than in most OECD countries, [66] and hospital occupancy has risen well above the desired 85% level. The King’s Fund is an independent charity founded more than 100 years ago that conducts research to improve health care in the UK. It released a recent report that suggested the greatest bottleneck is post-acute care, where after hospitalization, patients need medical support, either at home or in a specialized facility.
Intermediate (transitional) care capacity sits at about half the level of demand, while budget cuts have significantly reduced the availability of community-based long-term care beds, which are funded by local councils, outside the purview of the NHS. [67] Without expanded system capacity and a complementary policy, the 4-hour standard is insufficient to improve access.
A 2019 National task force failed to generate promising new strategies, and the UK government now favours a return to the 4-hour standard, but with a lower threshold of 76%. Even if achieved, the RCEM believes this target will not reduce ED crowding. Instead, its recommended solutions to ED crowding include prioritizing evidence-based interventions, improving hospital capacity and social services, ensuring the emergency medicine workforce is adequate, and introducing meaningful transparent performance metrics. [68]
Learnings
In the Canadian model of global budgets, every arriving patient is a cost to the hospital. More patients mean more stress on hospital resources. This creates an incentive to limit patient care and reduce access. [69]
We recommend that Canadian hospitals shift from global budgets with fixed funding envelopes and no embedded growth towards activity-based funding, which has become the international norm. Under this funding plan, every arriving patient is revenue. This motivates efficiency, flow, and throughput, allowing hospitals to expand capacity to better meet patient demand. [49] However, we also recommend reviewing the positive and negative international experiences with activity-based funding before incorporating it into the Canadian context. [70] Flow targets provide clarity around expectations and can drive operational improvement, but they are only surrogate quality measures, and may lead to gaming or compromising patient safety. [71,72,73] They remain essential, but must be thoughtfully and carefully incentivized.
Aged Care
|
CANADA I see an older patient who has become increasingly frail and is failing at home. With no community beds available, she waits 2 days on an ED stretcher and develops a delirium. On the inpatient ward, with little rehabilitation care, she becomes increasingly deconditioned. No longer a candidate for home care, she waits in hospital 6 more weeks for long-term placement. AUSTRALIA I see an older patient who has become increasingly frail and is failing at home. After 2 hours in the ED, I transfer her to the emergency short-stay unit where she rests and has tea. The care coordination team is unable to mobilize her and recommend admission. She stays in an acute medical bed for 20 days and is discharged to a rehabilitation centre. SWEDEN I join a geriatrics outreach team (geriatrician and two public health nurses) for a home visit. We visit an older person with dementia who lives with his wife in a comfortable, municipally supported 2-bedroom unit. He is in a wheelchair and his wife is making breakfast. The geriatrician assesses him while the nurses replace the dressings on his legs for peripheral edema, and draw bloodwork. Since his diagnosis of heart failure 2 years ago, the team has been able to prevent any potential visit to the local emergency department. |
System Overview
International long-term care (LTC) comparisons are difficult because of data limitations as well as variability in definitions and reporting of LTC beds. [74] However, we know that despite an aging population, Canada has invested less in LTC capacity than many countries, about 1.4% of GDP. [75] Sweden tops the list at just under 5% of GDP, while the UK and Australia stand at about 1.5% and 1.2% respectively. A recent international comparison suggests that England and Canada have the poorest access to LTC. [76] In addition to their lower public spending levels, these countries also rely less on client and family co-payments, and limit access based on the available LTC budget. In Australia, Canada, and the UK, care workers for the aged are in short supply and often poorly paid. [76,77,78]
Canada
Canada’s LTC facilities may be publicly or privately owned (for-profit or not-for-profit), [79] but they are publicly funded and regulated by provincial governments [80,81] with federal contributions. [82] Residents typically provide co-payments, with details varying widely by province. [83] Home care and community services represent approximately 6% of the health budget and are funded in a separate envelope; [84] services and co-payments, if applicable, also vary by province.
There are about 29 long term care (LTC) beds per 1,000 people over 65. [74] Long waits suggest that this is insufficient to meet demand: in 2021, more than 38,000 Ontarians were on a recent LTC waitlist, with a median wait time of 171 days. [85] Shortfalls in long term care also drive the Alternate Level of Care (ALC) phenomenon, in which patients who no longer require acute hospital care cannot be safely discharged, [86] and as a result, ALC patients, including those waiting for LTC, occupy 17% of Canada’s hospital beds. [87]
The Conference Board of Canada has determined that Canada will need 199,000 more LTC beds by 2035, a doubling of current capacity. This will cost an estimated $65 billion over the next 13 years, along with $130 billion in operating expenses. (2019 $CAD). While substantial, the benefits outweigh these costs, as it will unburden the hospital system, improve access to acute care, support 123,000 new jobs, and have a net positive effect on the economy. [88] However, it’s important to note that estimates are based on current patterns of care; innovations that enable more people to age at home may reduce the need for beds.
Australia
Aged care in Australia is under federal jurisdiction, [89] with services including care homes, short-term, respite, transitional care, and four levels of home care. [90] As in Canada, the government subsidizes aged care with an expectation of co-payment from residents. Not-for-profit, for-profit, and government providers deliver aged care services.
In 2008, [91] the most recent data indicated that the average waiting time for residential care was 24 days.
As of 2015, the country had 111 aged care spaces (81 residential and 30 home care) per 1000 people aged 70+ and aimed to raise this to 125 by 2021-22. [92]
In 2022, patients with alternate level of care needs occupied 6.5% of Western Australia hospital beds. [93] But since COVID-19, residential care has become less popular, and home care is now favoured, with the result that wait times for aging in place have increased.
Separate from their traditional home care services, Victoria and Tasmania make substantial use of Hospital in the Home, [94] a virtual ward that provides acute care for patients who are considered part of a hospital’s case mix. Each patient separation, or departure from hospital, is funded as an inpatient admission. A 2009 review revealed that one year of Hospital in the Home admissions (n=32,462) would have filled a 500-bed Australian hospital. [95] To support aged care, some regions have implemented virtual emergency services, and EMS residential outreach; [96] however, pre-existing GP support models within care homes also reduced ED transfers. [97]
Sweden
Under the Swedish Social Services Act, municipalities deliver aged care, funded by municipal taxes and government grants. [95] Municipalities must ensure that housing and residential areas accommodate older and disabled persons. A focus on enabling patients to live at home for as long as possible is a hallmark of the Swedish and other Scandinavian systems, combined with facility-based care as a last resort rather than a default option. [98,99]
Home services and special housing are provided publicly and privately, with a maximum copayment of 2,300SEK (about CAD$300) monthly, which is adjusted based on income. [100] Sweden has created mobile multi-disciplinary geriatric teams for complex older persons who need more services, along with transitional units with physician oversight, and community ambulance nurses specifically trained to care for older persons.
Municipalities have only three days to transfer hospitalized ALC patients back into the community. If this goal is not met, the municipality pays the additional hospital costs; [101] as a result, Swedish hospitals have few ALC patients.
Learnings
We support the Conference Board of Canada’s conclusions that large investment in LTC is necessary. This should begin immediately and continue as a 10- to 15-year health system priority. There is room for stronger federal input, particularly if this comes with funding, interprovincial standardization, and national strategic planning.
We recommend immediate investment in LTC transition capacity to address crippling ALC levels. This would:
- Expedite hospital outflow.
- Mitigate acute care and emergency access block.
- Decrease unit costs for ALC patients now stranded in acute hospitals.
- Improve rehabilitation and functional outcomes for older patients.
These units should be based on population needs, and reserved for their intended purpose—otherwise, they become holding units that fill up rapidly, yielding no benefit. [102] To prevent hospital transfers, LTC programs should introduce virtual support services, and partner with community paramedics to provide unscheduled care.
Substantial home care and LTC investment is critical, but should not occur without associated accountability expectations, including the extension of overcapacity protocols to the hospital–community transition (see Section 3: Accountability).
Canada should shift further towards the Scandinavian model of aging in place, offering a menu of subsidized home-based and residential services at different levels of intensity. Resident/family co-payments should be set in a way that is consistent and equitable across residential care settings; increasing the role of co-payments may be appropriate where the alternative is self-funded housing, and where fees are income-adjusted to ensure equity.
We should not necessarily adopt Sweden’s municipal model; after all, a municipal model also exists in the UK, but underfunding and poor integration with the NHS make it more of a hindrance than a help. However, Canada should consider introducing mechanisms that allow money to follow the patient to the most appropriate location along the continuum of care. Processes should also integrate the governance and operations of acute and community care programs to ensure a smooth transition of care.
Private vs. Public Healthcare
|
CANADA I encounter an active 76-year-old patient who twisted her right knee playing pickleball. She arrives with medial swelling and a limp. After assessing the injury, I diagnose her with a medial ligament sprain and possible meniscal tear. I refer her to a publicly-funded sports clinic where she can follow up with a physician, and acquire further imaging if needed. Because she’s over the age of 65, she’s eligible for publicly-funded physiotherapy (but it may take a few weeks) and I provide a list of outpatient clinics. If she wants to be seen faster, she can pay for physiotherapy privately. AUSTRALIA I encounter an active 76-year-old patient who twisted her right knee playing pickleball. She arrives with medial swelling and a limp. After assessing the injury, I diagnose her with a medial ligament sprain, possible meniscal tear, and refer her back to her primary care provider who can arrange further imaging and physio, as required. However, she tells me she cannot manage at home, and requests that I contact her orthopedic surgeon. The surgeon admits her to the private hospital for an MRI. I had earlier tried to transfer a patient with dementia and heart failure to the same hospital. The transfer was refused because of the patient’s comorbidities. UNITED KINGDOM I encounter an active 76-year-old patient who twisted her right knee playing pickleball. She arrives with medial swelling and a limp. After assessing the knee, I diagnose a medial sprain, possible meniscal tear, and recommend follow-up with her primary care provider who can arrange imaging and physiotherapy. She states she cannot access her primary care provider, and there’s a 6-month wait to see a physiotherapist. I advise that she can access a private orthopedic specialist or physiotherapist faster at her own expense. |
Canada
Many argue that Canada should allow privatized healthcare, as other countries do, to offload public demand and improve access for all. However, evidence suggests this approach may bleed resources from the public system, improving access for those able to pay, but leave public wait times unchanged. [102] In discussing this, we must distinguish financing (who pays) from delivery (who gets paid).
The Canada Health Act mandates public financing of medically-necessary physician and hospital services, but other healthcare is financed privately or through a mix of public and private financing. This includes drugs delivered outside hospital, services by non-physicians, outpatient dentistry, most long-term care, and procedures not deemed medically necessary, such as cosmetic surgery. Presently about 30% of Canadian healthcare is financed out-of-pocket or through private insurance. Each province has some form of Pharmacare, [103] but have high patient co-payments and/or co-insurance. This is in contrast to both Australia (104) and the UK, [105] where drug benefit programs are national and heavily subsidized.
Care delivery is also largely private. Many clinics are privately-owned, and most physicians are self-employed contractors who determine when they work, how much they earn, and what patients they see. There’s high corporate involvement in for-profit pharmacies and long-term care facilities. Most concerning is that companies have moved into the provision of virtual urgent care which generates more health cost but unclear value. [106] Some provinces use private for-profit clinics to address elective surgical backlogs, such as cataract surgery. [107]
Is Private Better?
Will private care delivery offload the public system? It is unclear. Private facilities can mobilize resources quickly and may add care capacity, but private delivery, especially by corporations, carries risk. There is evidence that for-profit hospitals and nursing homes deliver poorer-quality care. [108,109] Private clinics tend to skim high-volume, low-complexity (high profit) work, and some offer privately-financed options that bend or breach Medicare principles. Private facilities also poach staff from the public system. Since COVID-19, provider shortfalls, high workloads and stress, job-related burnout, and relatively low wages have driven many providers—particularly nurses—to private agencies where they have more control, better hours, and higher wages. Hospitals are then forced to re-hire these agency nurses, paying them higher wages as well as agency profit margins. [110] Canadian nurses are also finding higher pay and better hours in the USA, [111] leaving understaffed Canadian hospitals, ED closures, longer patient waits and greater stress on those left behind. [112] Privatization introduces market forces that may be good for providers, but bad for patients and public financing. It seems inevitable, however, that privatization will increase over time.
Australia
In Australia, rural and remote care, academic medicine, and complex cases are concentrated in public hospitals. However, 40% of hospitalizations, 60% of surgical admissions (mostly elective), and 1% of emergency admissions are to private hospitals. [113,114] Private (for-profit and not-for-profit) hospitals charge patients and their insurance carriers and receive government subsidies for insured services. [113] These hospitals tend to skim “easy” patients and transfer those with more complex conditions to public hospitals. Conversely, public hospitals purchase capacity from private hospitals for patients who are low-complexity, insured, and convalescing. [114]
Long public wait times drive patients into the private system, which provides Australians a choice but creates inequity. [115] Better compensation also draws providers to private settings, [114,115,116] but private hospitals do not provide full-spectrum care, so system integration and planning are weakened, and subsidies provide less return on investment. [114] Private surgical care could reduce public wait times if it increased surgical capacity by adding surgeons or operating time. But if it shifts surgical capacity (surgeon time) from public to private settings, it will not shorten public wait times, and it has not. [114,116]
United Kingdom
Despite universal healthcare, 10% of the UK population has private health insurance, either self-funded or through employment. [117] This is primarily to access elective or specialized care when waiting times are long, and it creates inequity. The UK government uses private healthcare to reduce wait times for elective surgery (such as hip replacement) and diagnostic imaging (eg CT or MRI), in the hope of increasing inpatient bed capacity. Based on the ability to pay, patients with urgent, emergent needs, low complex issues or day surgery can access NHS or private care. But complex patients with less urgent problems who need an inpatient bed may face long waits for treatment in NHS facilities; this is because private providers tend to choose simpler cases. Unintended consequences abound. For example, specialties that can provide private care are more attractive, and patients often pay higher rates to have problems addressed by private doctors, sometimes in NHS facilities. Patients with the ability to pay for outpatient care, such as physiotherapy, may do so.
A Word About the American Healthcare System
Explorations of what Canada can learn from other health systems is often meet with resistance, for both good and bad reasons. The good is that we can’t simply import another country’s health system without also importing its history and culture; nor can we expect to find a magic bullet among the myriad features and initiatives that happen to exist abroad. The bad reason relates to the fear that looking beyond our borders means looking south to the heavily-privatized American system.
Based on inequities, the USA scores dead last in Commonwealth Fund comparisons, administrative inefficiencies and ballooning costs of its multi-payer system. [5] This is why we did not include it in our comparative discussion. However, there are models of care within the US, such as the not-for-profit Intermountain Healthcare, [118] from which we can learn. Intermountain Healthcare is the pioneer of incorporating quality improvement into clinical care as a Learning Health System. [119])
Learnings
All 38 countries in the OECD (Organisation for Economic Co-operation and Development), including Canada, have private delivery of publicly-funded health services.
Canada differs from Australia and the UK (and all other OECD countries) in that private, for-profit hospitals aren’t allowed under the Canada Health Act. Conversely, Canada also has more privatization in some sectors, such as Pharmacare and long-term care, when compared to Australia, UK, or Sweden. While private hospitals offer the promise of decanting patients from an overburdened public system, they also have a deleterious impact on the health workforce and exacerbate societal inequities. Highly-privatized systems do not fulfill the equity facet of the Quintuple Aim, which makes them incompatible with Canadian values.
Our current healthcare system is not nearly as accessible as it should be, does not consistently achieve patient or provider satisfaction, and has mixed population outcomes. Until we do better on these measures there will continue to be conflict between those calling for more privatization and those defending the promise of Medicare. There is another way, but a critical part of the Canadian healthcare redesign puzzle requires us to be a Learning Health System, [4] one that’s open to the experience of others and balances the best of all systems in pursuit of the Quintuple Aim. [120]
Recommendations: Lessons from Other Healthcare Systems
Canada has a relatively poor-performing healthcare system, and we can learn from others. Our review of international practices suggests that high-performing systems are more centralized, integrated, and collaboratively managed than Canada. There are no magic bullets, but several potential innovations are highlighted in the list below:
- Develop a national workforce strategy with strong federal input using a standardized approach to data, measurement, integration, and prediction.
- Eliminate interprovincial mobility barriers.
- Increase physician capacity, primarily through medical school expansion, targeting the OECD average of 3.6 per 1000 population with appropriate distribution matching population needs.
- Introduce market-based incentives to attract physicians to practice in areas of most need (e.g. generalist-specialist mix, marginalized populations, and rurality).
- Encourage health professionals, including medical trainees, to work to full scope.
- Increase peer-to-peer support by telemedicine for rural physicians.
- Shift away from global hospital budgets toward activity-based funding, but tailor it to the Canadian system with appropriate guardrails.
- Under an accountability framework, develop system-wide flow targets aimed at improving access to long-term care, acute care, emergency care, diagnostic imaging, specialty access and primary care. Incorporate incentives that discourage gaming, and progress toward these targets in a graded fashion. We strongly recommend 85% hospital occupancy. Consider short-stay units that are not holding areas.
- Make long-term care the priority target for new spending but ensure this investment is linked to an accountability framework and performance measurement.
- Evolve toward an aging-at-home model. Consider increasing patient and family co-payments adjusted to ability to pay, and having home care patients considered part of a hospital’s case-mix for funding allocation.
- Add LTC transition spaces and community overcapacity beds that would serve as rapid intake buffer capacity to improve access to care and hospital outflow. Consider policies to incentivize rapid re-integration of hospitalized ALC patients back into the community.
- Introduce virtual support and community paramedics to augment home (and facility) care and reduce transfers to hospital.
- Implement overcapacity protocols that bridge the hospital-community outflow interface.
- Acknowledge the reality that provider compensation in the public system must be competitive with the private system.
- Consider privatization only in areas where evidence resulting from comprehensive comparisons with other healthcare systems suggests an improvement of patient and population outcomes. At a minimum, there should be no equity threats. If implemented, closely monitor the system for—and regulate response to—unintended consequences.
- Collaborate with international partners to develop more comprehensive international recommendations for health system improvement.
- Learn from and collaborate with other countries to be an effective Learning Health System.
References
- Canadian Medical Association. Recommendations for federal action to address Canada’s health care crisis. 2022 Feb 15;
- Martin D, Miller AP, Quesnel-Vallée A, Caron N, Vissandjée B, Marchildon GP. Canada’s universal health-care system: achieving its potential. The Lancet. 2018;391(10131):1718–35.
- Martin D. Better now: six big ideas to improve health care for all Canadians. Penguin; 2017.
- Foley T. FF. The Potential of Learning Healthcare Systems. 2015 Nov;
- The Commonwealth Fund. Mirror, Mirror 2021: Reflecting Poorly – Health Care in the U.S. Compared to other High-income countries. 2021 Aug 4;
- OECD iLibrary. Health at a Glance 2021: OECD Indicators – Doctors (overall number).
- OECD Data. Nurses. 2021;
- Government of Canada. Canada’s Health Care System.
- Office of the Auditor General of Ontario. Section 3.07 Funding Alternatives for Specialist Physicians. 2011;
- Ontario Ministry of Health. Health Workforce Planning Branch.
- Ministry of Health and Long-Term Care – Health Workforce Evidence and Innovation Unit. Health Professions Database 2013 Stat Book. 2016;
- Ontario Physician Reporting Centre. Physicians in Ontario 2021.
- Canadian Institute of Health Information. Health Workforce in Canada: In focus (including nurses and physicians). 2022 Nov 17;
- McQuillan L. Canada’s push to ‘poach’ nurses from abroad fuels fears of shortages in developing countries. 2022 Nov 20;
- Lapierre M. New Brunswick seeks nurses from Quebec amid health-care worker shortage. CBC News. 2023 Jan 24;
- Kanyigan J WR. Alberta looks to poach skilled workers from Vancouver, Toronto. CTV News – Calgary. 2022 Aug 15;
- Ontario Government – Office of the Premier. New “As of Right” Rules a First in Canada to Attract More Health Care Workers to Ontario. 2023 Jan 19;
- Alberga H. Ontario looking to poach health-care workers from other provinces to fill shortages. CTV News – Toronto. 2023 Jan 19;
- Collaborative Working Group on the Future of Emergency Medicine in Canada. Emergency Medicine Training and Practice in Canada: Celebrating the Past and Evolving for the Future. 2016;
- Philippon D, Marchildon G, Ludlow K, Boyling C, Braithwaite J. The comparative performance of the Canadian and Australian health systems. 2018; Healthcare Management Forum 31(6):239–44.
- Bourgeault I, Simkin S, Chamberland-Rowe C. Poor health workforce planning is costly, risky and inequitable. Cmaj. 2019;191(42):E1147–8.
- Crettenden IF, McCarty MV, Fenech BJ, Heywood T, Taitz MC, Tudman S. How evidence-based workforce planning in Australia is informing policy development in the retention and distribution of the health workforce. Human Resources for Health. 2014;12(1):1–13.
- Australian Government Department of Health. Future focused Primary Health Care: Australia’s Primary Health Care 10 Year Plan 2022-2032. 2022 Mar;
- Australian Government: Department of Health and Aged Care. Aged care workforce strategy.
- Australian Government: Department of Health and Aged Care. AGPT Program GP Workforce Planning and Prioritisation. 2021;
- Australian Government: Department of Health and Aged Care. Emergency Medicine – Australia’s Future Health Workforce report. 2017;
- Phillips J. Health workforce [Internet]. [cited 2023 Aug 17]. Available from: https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/BriefingBook46p/HealthWorkforce
- Vines E, Storen R. Health workforce [Internet]. [cited 2023 Aug 17]. Available from: https://www.aph.gov.au/About_Parliament/Parliamentary_departments/Parliamentary_Library/pubs/BriefingBook47p/HealthWorkforce
- Boniol M, Siyam A, Diallo K, Campbell J. Urgent need to invest in health and care workers. The Lancet. 2022;
- Daniel D. Train your own nurses, Australia told amid global shortage. The Sydney Morning Herald. 2022 Jul 29;
- Waters A. A third of junior doctors plan to leave NHS to work abroad in next 12 months. 2022;
- Australian Nursing & Midwifery Federation. Australia criticised for poaching nurses from low-income countries. 2022 Oct 17;
- Parliament of NSW Legislative Council. Impact of ambulance ramping and access block on the operation of hospital emergency departments in New South Wales. 2022 Dec;
- Australasian College for Emergency Medicine. Constructing and Retaining a Senior Emergency Medicine Workforce. 2021 Nov;
- Baker T, Moore K, Lim J, Papanastasiou C, McCarthy S, Schreve F, et al. Rural emergency care facilities may be adapting to their context: A population-level study of resources and workforce. Aust J Rural Health. 2022 Jun;30(3):393–401.
- My Emergency Doctor. Virtual board rounds reducing clinical risk and improving operational outcomes. 2022 Oct 14;
- International Federation of Emergency Medicine. An Updated Framework on Quality and Safety in Emergency Medicine, 2nd Edition. 2019 Jan;
- Sri-Ganeshan M, Cameron P, O’Reilly G, Mitra B, Smit D. Evaluating the utility of telehealth in emergency medicine. Emergency Medicine Australasia. 2022;34(6):1021–4.
- Savage D PD. LO77: Assessing the long-term emergency physician resource planning for Nova Scotia, Canada. Canadian Journal of Emergency Medicine. 2019;21(S1):S35-36.
- Islam R, Kralj B, Sweetman A. Physician workforce planning in Canada: the importance of accounting for population aging and changing physician hours of work. CMAJ. 2023;195(9):E335–40.
- Cheng I, Taylor D, Schull MJ, Zwarenstein M, Kiss A, Castren M, et al. Comparison of emergency department time performance between a Canadian and an Australian academic tertiary hospital. Emerg Med Australas. 2019 Aug;31(4):605–11.
- Ontario Medical Association. Fact Sheet: Canada Health Transfer Payments. Prescription for Ontario: Doctor’s 5-Point Plan for Better Health Care. 2021 Oct 26;
- Hewett R. Public hospital funding: an overview [Internet]. [cited 2023 Aug 17]. Available from: https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/FlagPost/2022/July/Hospital-funding
- National Health Funding Body. Local Hospital Networks – National Health Funding Body [Internet]. National Health Funding Body; 2023 [cited 2023 Aug 17]. Available from: https://www.publichospitalfunding.gov.au/public-hospital-funding-reports
- Health at a Glance 2021: OECD Indicators – Hospital Beds and Occupancy [Internet]. OECD; 2021 [cited 2023 Aug 17]. (Health at a Glance). Available from: https://www.oecd-ilibrary.org/sites/e5a80353-en/index.html?itemId=/content/component/e5a80353-en
- World Bank – Data. Current health expenditure per capita (current US$). 2022 Jan 30;
- Sutherland JM, Liu G, Crump RT, Law M. Paying for volume: British Columbia’s experiment with funding hospitals based on activity. Health Policy. 2016 Nov;120(11):1322–8.
- Laberge M, Brundisini FK, Champagne M, Daniel I. Hospital funding reforms in Canada: a narrative review of Ontario and Quebec strategies. Health Research Policy and Systems. 2022;20(1):1–17.
- Sutherland J RN. Current Hospital Funding in Canada Policy Brief. Vancouver: UBC Centre for Health Services and Policy Research. 2014.
- Ontario Hospital Association. Health-Based Allocation Model (HBAM): What you Need to Know.
- Ontario Ministry of Health. Health System Reform.
- Kreindler SA. Planning without action and action without planning? Examining a regional health system’s efforts to improve patient flow, 1998-2013. Int J Health Plann Manage. 2018 Jan;33(1):e333–43.
- Cheng AHY, Sutherland JM. British Columbia’s pay-for-performance experiment: part of the solution to reduce emergency department crowding? Health Policy. 2013 Nov;113(1–2):86–92.
- Vermeulen MJ, Stukel TA, Boozary AS, Guttmann A, Schull MJ. The Effect of Pay for Performance in the Emergency Department on Patient Waiting Times and Quality of Care in Ontario, Canada: A Difference-in-Differences Analysis. Ann Emerg Med. 2016 Apr;67(4):496-505.e7.
- Independent Hospital Pricing Authority. Health Policy Analysis: Australian Emergency Care Classification: Definitions Manual. 2019;
- Silk K. The National Emergency Access Target: aiming for the target but what about the goal? 2016 Apr 26;
- Nahidi S, Forero R, Man N, Mohsin M, Fitzgerald G, Toloo GS, et al. Impact of the Four-Hour Rule/National Emergency Access Target policy implementation on emergency department staff: A qualitative perspective of emergency department management changes. Emerg Med Australas. 2019 Jun;31(3):362–71.
- Forero R, McCarthy S, Hillman K. Access block and emergency department overcrowding. Crit Care. 2011;15(216):1–6.
- Hession M, Forero R, Man NW, Penza L, McDonald W. Gaming National Emergency Access Target performance using Emergency Treatment Performance definitions and emergency department short stay units. Emerg Med Australas. 2019 Dec;31(6):997–1006.
- Forero R, Man N, Nahidi S, Fitzgerald G, Fatovich D, Mohsin M, et al. When a health policy cuts both ways: Impact of the National Emergency Access Target policy on staff and emergency department performance. Emerg Med Australas. 2020 Apr;32(2):228–39.
- Frommer M MS. Access block: A review of potential solutions. Sax Institute, editor. 2022.
- O’Reilly J, Busse R, Häkkinen U, Or Z, Street A, Wiley M. Paying for hospital care: the experience with implementing activity-based funding in five European countries. Health Econ Policy Law. 2012 Jan;7(1):73–101.
- Locker TE, Mason SM. Are these emergency department performance data real. Emerg Med J. 2006 Jul;23(7):558–9.
- Mason S, Weber EJ, Coster J, Freeman J, Locker T. Time patients spend in the emergency department: England’s 4-hour rule-a case of hitting the target but missing the point? Ann Emerg Med. 2012 May;59(5):341–9.
- Nuffield Trust. Ambulance Handover Delays. 2023 Apr 27;
- Boyle A HI. RCEM Acute Insight Series: Crowding and its Consequences. Royal College of Emergency Medicine, editor. 2021 Nov;
- Ewbank L, Thompson J, McKenna H, Anandaciva S, Ward D. The King’s Fund. 2021 [cited 2023 Aug 17]. NHS hospital bed numbers. Available from: https://www.kingsfund.org.uk/publications/nhs-hospital-bed-numbers
- Royal College of Emergency Medicine. Resuscitating Emergency Care.
- Sutherland J TCR. Paying for Hospital Services: A Hard Look at the Options. C.D. Howe Institute; 2013.
- Palmer KS, Agoritsas T, Martin D, Scott T, Mulla SM, Miller AP, et al. Activity-Based Funding of Hospitals and Its Impact on Mortality, Readmission, Discharge Destination, Severity of Illness, and Volume of Care: A Systematic Review and Meta-Analysis. PLOS ONE. 2014 Oct 27;9(10):e109975.
- Hardern RD. The 4-h target: an example of destructive goal pursuit. Emerg Med J. 2012 Mar;29(3):219–21.
- Keijzers G. NEAT in need of a sweet spot. 2014.
- Sikka R, Morath JM, Leape L. The Quadruple Aim: care, health, cost and meaning in work. 2015.
- Canadian Institute of Health Information. How many long-term care beds are there in Canada? 2021 Jun 10;
- Dyer S. VM. Review of International Systems for Long-Term Care of Older People: Report prepared for the Royal Commission into Aged Care Quality and Safety: research paper 2. 2019;
- Committee of Economic Development Australia. Australia’s Dire Shortage of Aged-Care Workers Requires Immediate Action: CEDA. 2021 8;
- Zagrodney K, Deber R, Saks M, Laporte A. The Disadvantaged Home Care Personal Support Worker: Differences in Job Characteristics, Unionization, Pensions, Participation, and Wages by Care Sector in Canada. J Appl Gerontol. 2023 Apr 1;42(4):758–67.
- Foster D. Adult social care workforce in England. 2023 Aug 18 [cited 2023 Aug 17]; Available from: https://commonslibrary.parliament.uk/research-briefings/cbp-9615/
- Canadian Institute of Health Information. Long-term care homes in Canada: How many and who owns them? 2021 Jun 10;
- Ontario Long Term Care Association. Long Term Care – Facts and Figures.
- Ontario Ministry of Long Term Care. Ministry of Long Term Care.
- Canadian Association for Long Term Care. What is long-term care? 2022;
- Kreindler SA, Aliyu G, Conrad D, Parveen S. Structural and population features of Western Canada’s urban health regions and zones. Center for Healthcare Innovation; 2015.
- Expert Group on Home and Community Care. Bring Care Home. 2015 Mar;
- Ontario Government. Ontario Welcomes New Long-term Care Development Proposals. 2021 Oct 20;
- Canadian Institute of Health Information. Guidelines to Support ALC Designation.
- Canadian Institute of Health Information. Hospital Stays in Canada. 2023 Feb 23;
- R Gibbard. Sizing up the challenge: Meeting the demand for long-term care in Canada. Conference Board of Canada, editor. Canadian Economics. 2017 Nov 27;
- Australian Government Department of Health and Aged Care. Aged Care.
- Australian Government Department of Health and Aged Care. My Aged Care.
- Australian Government: Australian Institute of Health and Welfare. Movement from hospital to residential aged care. 2008 Nov 26;
- Grove A. Aged Care: A Quick Guide. Parliament of Australia, editor. 2016 Oct 24;
- Office of the Auditor General Western Australia. Management of Long Stay Patients in Public Hospitals. 2022 Nov 16;
- Victoria Department of Health. Hospital in the Home.
- Montalto M. The 500‐bed hospital that isn’t there: the Victorian Department of Health review of the Hospital in the Home program. Medical journal of Australia. 2010;193(10):598–601.
- Northern Health. Victorian Virtual Emergency Department.
- Pain T, Stainkey L, Chapman S. AgedCare+GP: description and evaluation of an in-house model of general practice in a residential aged-care facility. Aust J Prim Health. 2014;20(3):224–7.
- Colombo F. LNA. Help Wanted? Providing and Paying for Long-Term Care, OECD Health Policy Studies. OECD, editor. 2011;
- Health at a Glance 2015: OECD Indicators. 2015;
- Swedish Government. Elderly care in Sweden: Sweden’s elderly care system aims to help people live independent lives. 2022 May 2;
- Region Orebro Ian. 1177 Vardguiden: Patientavgifter och hogkostnadsskydd.
- Kreindler SA, Struthers A, Star N, Bowen S, Hastings S, Winters S, et al. Can facility-based transitional care improve patient flow? Lessons from four Canadian regions. Healthc Manage Forum. 2021 May;34(3):181–5.
- Brandt J, Shearer B, Morgan SG. Prescription drug coverage in Canada: a review of the economic, policy and political considerations for universal pharmacare. J Pharm Policy Pract. 2018;11:28.
- Care AGD of H and A. Pharmaceutical Benefits Scheme (PBS) | About the PBS [Internet]. Australian Government Department of Health and Aged Care; [cited 2023 Aug 18]. Available from: https://www.pbs.gov.au/info/about-the-pbs
- uk [Internet]. 2020 [cited 2023 Aug 18]. NHS prescription charges. Available from: https://www.nhs.uk/nhs-services/prescriptions-and-pharmacies/nhs-prescription-charges/
- Innes G. Fast food medicine. Canadian Journal of Emergency Medicine. 2023;1–2.
- Canadian Broadcasting Corporation. Doug Ford Government will give for-profit clinics bigger role in surgeries. 2023 Jan 13;
- Stall NM, Jones A, Brown KA, Rochon PA, Costa AP. For-profit long-term care homes and the risk of COVID-19 outbreaks and resident deaths. CMAJ. 2020 Aug 17;192(33):E946–55.
- Ontario Health Coalition. The Horrifying Truth about For-Profit Long Term Care Homes. 2021 Dec 1;
- Laucius J. ‘It’s corrosive. They’re price gouging:’ Agency staffing is costing hospitals, LTC homes, critics say. Ottawa Citizen. 2022 Aug 18.
- Woodward J. Nurses Leaving Canada Double in the last Five Years amid Health-care Crisis. CTV News, editor. 2022 Oct 26.
- Kampf S. A. Inside ERs at a breaking point, staff provide care while juggling shortages and closures. Canadian Broadcasting Corporation, editor. 2022 Oct 2.
- Australian Government: Australian Institute of Health and Welfare. Australia’s Hospitals at a Glance. 2022 Dec 7.
- Duckett S. Commentary: the consequences of private involvement in healthcare–the Australian experience. Healthcare Policy. 2020;15(4):21.
- Duckett SJ. Living in the parallel universe in Australia: public Medicare and private hospitals. Cmaj. 2005;173(7):745–7.
- Duckett SJ. Private care and public waiting. Australian Health Review. 2005;29(1):87–93.
- Vankar P. Percentage of population covered by public or private health insurance in the United Kingdom from 2000 to 2019. Statista, editor. 2023 Mar 1;
- Home – Intermountain Health [Internet]. [cited 2023 Aug 18]. Available from: https://intermountainhealthcare.org/
- 4 Steps to a Learning Healthcare System [Internet]. [cited 2023 Aug 18]. Available from: https://intermountainhealthcare.org/blogs/4-steps-to-a-learning-healthcare-system
- Nundy S, Cooper LA, Mate KS. The Quintuple Aim for Health Care Improvement: A New Imperative to Advance Health Equity. JAMA. 2022 Feb 8;327(6):521–2.
