It starts but must not end here. A single report will not change the trajectory of health care in Canada. Leading large-scale change is a continuous process, initiated by the impetus to make positive change and fed by a continuous cycle of consultation, engagement, and improvement.
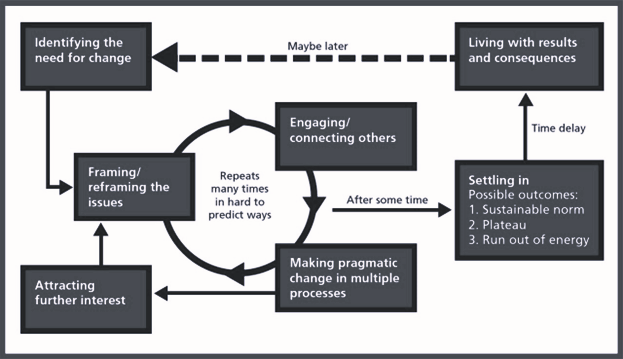
Figure 21. The Leading Large Scale Change model that has guided our work, and should influence future strategies, both locally and at scale. (NHS England Sustainable Improvement Team, 2017.)
EM:POWER’s underlying assumption is that the entire emergency medicine system must be better integrated and aligned to the needs of our patients and populations to optimize its role in achieving the Quintuple Aim.
This report’s recommendations and change strategies are not just theoretical, but can be applied at local, regional, and national levels across Canada to pave the way for a more efficient, patient-centered, and resilient emergency care system.
Essential redesign aspects of a high-functioning health ecosystem have been explored and include:
- Optimizing access points to emergency care within integrated clinical networks (a reference point for addressing unexpected ED closures and workforce challenges)
- Creating accountability frameworks to address system-wide access block (a reference point for ED crowding)
- Disaster, pandemic, and surge preparedness, as well as system and workforce readiness and resilience (a reference point for the daily and weekly surges we experience in our EDs), and
- Adapting and evolving to a changing world and advancements in knowledge, by becoming a Learning Health System.
These findings have been shared with all Provincial and Territorial Ministers and Deputy Ministers of Health at their respective fall meetings. CAEP subsequently proposed that the Provincial and Territorial Ministers support a national forum, which would allow for health leaders, stakeholders, and policymakers to build on the momentum of the EM:POWER project, and use its evidenced-based recommendations as a framework for system change in the following areas:
- Facilitate the exchange of best practices, successful strategies and lessons learned from across the country
- Promote collaboration among emergency care providers, policymakers, administrators, decision-makers and other stakeholders
- Promote the establishment of care networks to coordinate clinical services and workforce planning
- Identify and propose system-wide policy recommendations centering around accountability frameworks, to help alleviate ED crowding and improve patient outcomes
- Identify pilot initiatives that can be trialed/adopted where needed in Canada
- Identify potential champions across the country to initiate change, and
- Establish consensus on how best to move forward on a continuing basis to further system redesign and help achieve the Quintuple Aim.
We look forward to hearing from the Ministers and working with them collaboratively to build a better emergency care system within a redesigned health ecosystem that will benefit all Canadians.
References
- Grumbach K. Redesign of the health care delivery system a Bauhaus, “Form Follows Function” approach. JAMA. 2009;302(21):2363–4.