Acquired hemophilia A
Presentations of rare bleeding disorders (RBDs) have a low incidence rate and therefore we, as emergency department (ED) physicians, may not be as familiar with these clinical scenarios, which can be subtle and require high clinical acumen to detect.
Acquired hemophilia A (AHA) is both rare and life threatening, and affects 1.3–1.5 million people each year, with 70% of these individuals experiencing a life-threatening bleed that may lead to death (22% mortality rate).1 This autoimmune disease is caused by autoantibodies to factor VIII (8) (FVIII), resulting in FVIII deficiency and a bleeding tendency. Occurrence of primary and secondary AHA is idiopathic more than 50% of the time, and the incidence is increased among postpartum women and among elderly men and women
In post-partum women, AHA tends to present one to four months after childbirth. Common features of post-partum AHA include severe ecchymosis, soft tissue hematomas, hemarthrosis, and severe life-threatening hemorrhage.2 In elderly patients with AHA, there are no differences observed in the distribution of the disease across sexes and it typically presents in patients with no prior history of bleeding.3
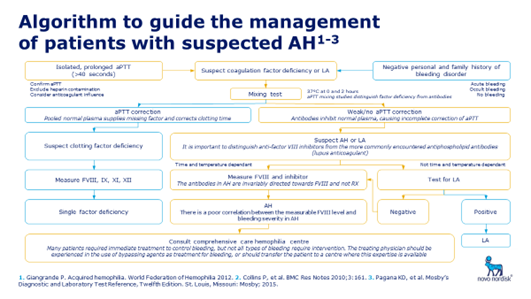
Higher awareness of AHA may lead to earlier diagnosis and improved outcomes. ED physicians are in a unique position to affect outcomes by identifying AHA quickly and implementing a treatment plan with your local referral network. In the ED, AHA should be considered when there are signs of easy bruising or bleeding, and whenever an acute or recent onset of bleeding is accompanied by an unexplained, prolonged activated partial thromboplastin time (aPTT).4 To assist with the categorization of bleeding, the Canadian Emergency Department Triage and Acuity Scale has classified triage of bleeding disorders as Level II or III depending on bleeding severity9. Routine lab tests (e.g., complete blood count [CBC], prothrombin time [PT] and aPTT) may help to detect AHA and if suspected, a consult with a hematologist is required.
IMAGE:
The objectives for AHA management include the following:
- Control and prevention of bleeding (if present or significant)
- Treatment of the underlying disease (if applicable)
- Eradication of the inhibitor
For AHA patients with active bleeding or risk of bleeding (prophylaxis of bleeding), individualized therapy should center around hemostatic control (i.e. the use of by-passing agents such as rFVIIa, aPCC and/or recombinant porcine factor VIII) to stop the bleeding, and the use of immunosuppressive agents for elimination/removal of autoantibodies to obtain stable and complete remission). However, AHA patients are susceptible to immunosuppression and severe adverse events. Therefore, the choice of therapy should be individualized and depends on the following:
- Inhibitor titre and FVIII level
- Bleeding pattern (e.g., location, severity, etc.)
- Estimated duration of therapy (dependent on prognostic factors)
- Planned other therapy (e.g., immunoadsorption)
- Patient condition and comorbidity (including current medications)
- Availability of medication and pharmacoeconomics
Avoidance of invasive procedures will reduce the complications for massive bleeding and save costs.
Tile Front
- Patient presents to ED with epistaxis that won’t stop bleeding
- Past medical history:
- Not taking any anticoagulation medication
- No family history of bleeding disorders
Examination
- E.g., Blood pressure
- Pulse
 5-7
5-7
Actions
Initial Management
- E.g., stabilize patient
Controlling Epistaxis8
Instruct the patient:
- To gently blow the nose to remove mucous and unstable clots, which will interfere with hemostasis.
Mucous membrane bleeding
- Tilt the head forward so any blood will come out the nares and not down the back of the throat.
- Apply firm pressure to the entire side of the nose that is bleeding for 15 minutes.
- Release the pressure to see if bleeding has stopped, blow out any soft clots.
- If the bleeding continues, reapply pressure for another five minutes.
- Factor replacement* at a routine dose and/or anti-fibrinolytic agents may be needed.
- During active bleeding, or when the bleeding has stopped, spray or apply two drops of oxymetazoline (e.g., NeoSynephrine®, Dristan®, or Afrin®) nasal spray/drops to the side that was bleeding. These can be used at home PRN for epistaxis.
- Instruct the patient to use olive oil in the nares to keep the membranes soft and moist, and to prevent the formation of hard crusts that might crack and restart bleeding.
- An ENT consult may be required for possible cauterization of a vessel.
Investigation
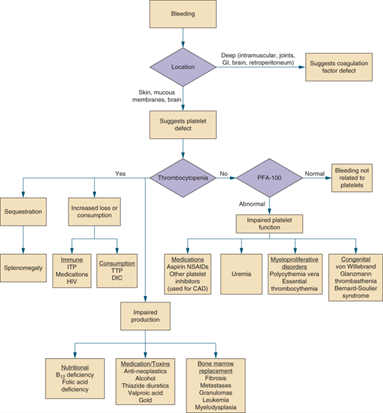
Easy bruising and bleeding may be signs of an underlying disorder.
CBC, PT, and aPTT are routine tests that may be used to detect some, but not all, bleeding disorders.
- aPTT should be ordered in addition to a PT/INR in cases of a suspected bleeding disorder.1,2
- PT/INR is used to monitor the extrinsic clotting cascade.3
- aPTT serves as screening test to identify coagulation disorders affecting the intrinsic clotting cascade, such as hemophilia.3
Order aPTT in cases of:
- Unexplained bruising
- Prolonged postsurgical bleeding
- Post-dental procedure bleeding
- Soft tissue or muscle bleeding from minor or no trauma
- Intracranial bleeding
Consult a hematologist if a bleeding disorder is suspected.
Supportive Management
- Monitoring of WBCs, platelets, hemoglobin, blood glucose, infections, mental changes, etc.
- Start of low molecular weight heparin (LMWH) for prophylaxis of thromboembolism when FVIII begins to rise.
Practice Considerations
- Guidelines recommend that AHA be considered whenever an acute or recent onset of bleeding is accompanied by unexplained, prolonged APTT.4
- Testing for FVIII activity and inhibitor concentration using the Bethesda assay and/or an anti-FVIII ELISA assay is recommended to confirm a diagnosis of AHA.4
Treatment
- Pharmacologic treatment options include hemostatic treatments and immunosuppressive treatments (ISTs).4
- Current hemostatic treatment options for AHA include rFVIIa (recombinant activated factor VII), pd-APCC (plasma derived activated prothrombin complex concentrate, and rpFVIII (recombinant porcine factor VIII).4
- Current IST treatment options for AHA include steroids, cyclophosphamide, and rituximab.4
Acronyms
APCC: Activated prothrombin complex concentrate
ED: Emergency department
ENT: Ear, nose, and throat specialist
INR: International normalized ratio
PNR: As needed
WBCs: White blood cells
References
- Centers for Disease Control. What is Hemophilia? 2020. Available at: https://www.cdc.gov/ncbddd/hemophilia/facts.html. Retrieved November 10, 2020.
- Seethala S, et al. Postpartum Acquired Hemophilia: A Rare Cause of Postpartum Hemorrhage. 2013;2013.
- Yousphi AS, et al. Acquired Hemophilia A: A Rare but Potentially Fatal Bleeding Disorder. Cureus. 2019;11(8):e5442.
- Tiede A, et al. International recommendations on the diagnosis and treatment of acquired hemophilia A. Haematologica. 2020;105(7):1791-1801.
- Collins P, et al. Consensus recommendations for the diagnosis and treatment of acquired hemophilia A. BMC Research Notes. 2010;3(1):161.
- Giangrande P. Acquired Hemophilia. 2012. Available at: http://www1.wfh.org/publications/files/pdf-1186.pdf. Retrieved November 10, 2020.
- Pagana K, et al. Mosby’s Diagnostic and Laboratory Test Reference. 13th ed; 2016.
- Wulff K, et al. Emergency Care for Patients with Hemophilia: An instructional manual for Medical Professionals. 3rd ed; 2018.
- Bullard MJ, et al. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) Guidelines 2016. CJEM. 2017;19(S2):S18-S27.
Bleeding disorders introduction/general practice
Introduction:
Bleeding disorders:
Congenital bleeding disorders are genetic disorders characterized by a deficiency or absence of one of the clotting proteins in the plasma, which results in in delayed clotting. Acquired bleeding disorders are not caused by genetic abnormalities and may present later in life.
Hemophilia:
Deficiencies of factor VIII (8) [Hemophilia A or Classic Hemophilia] and factor IX (9) [Hemophilia B or Christmas Disease] are the most common forms of bleeding disorders and are commonly referred to as hemophilia. Persons with hemophilia do not bleed faster than others; rather the bleeding is continuous. Significant blood loss can occur if treatment is delayed.
Hemophilia mostly affects males due to the X-linked inheritance pattern. The incidence of Hemophilia A worldwide is estimated to occur in 1:5,000 live male births, while Hemophilia B is more rare with an incidence of 1:25,000 live male births; all ethnicities are equally affected. Factor VIII deficiency is four times more common than factor IX deficiency but the clinical presentations and inheritance patterns are similar.1
Severity
The severity of bleeding expected in an individual with hemophilia depends upon the severity of the deficiency. Normal plasma levels of factor VIII and IX in non-hemophilic individuals range from 50–150%.
- Severe hemophilia: Those with less than 1% factor VIII and IX are considered to have severe hemophilia. Frequent bleeding episodes are common, particularly into joints. Bleeding can occur for unknown reasons (spontaneous bleeding) or due to trauma. Spontaneous bleeding is most common in severe hemophilia.
- Moderate hemophilia: Persons with factor levels of 1–5% are considered to have moderate hemophilia. These persons experience bleeding after trauma and less commonly for unknown reasons.
- Mild hemophilia: Persons with 5% – < 40% factor activity are considered to have mild hemophilia and bleed only after significant trauma or with surgery.
Basics
Serious bleeding sites
The six major sites of serious bleeding which threaten life, limb, or function are:
- intracranial
- spinal cord
- throat
- intra-abdominal
- limb compartments
- ocular
All of the above require immediate assessment and intervention, and are characterized by:
- bleeding into an enclosed space
- compression of vital tissues
- potential loss of life, limb, or function
Female Hemophilia Carriers:
Women can also be affected by hemophilia and other bleeding disorders. Women can be hemophilia carriers (i.e., have a genetic mutation on one of their X chromosomes resulting in abnormal factor VIII or IX), and like males, some will display symptoms depending on their factor levels. The level of factor activity determines the bleeding tendency and severity of symptoms in female carriers. Approximately 20% of carriers are symptomatic to some degree, while the remaining proportion of carriers display no symptoms (called asymptomatic carriers).2
Von Willebrand Disease (VWD):
- VWD is the most common congenital bleeding disorder with a prevalence of 1:100 to 1:1000 and affects both men and women
- Bleeding symptoms can vary depending on severity and type of VWD
- Bleeding symptoms are commonly mucocutaneous (e.g., epistaxis, gingival, gastrointestinal, genitourinary, uterine/menorrhagia) and can occur with invasive procedures (e.g., dental extractions, surgery) and childbirth
- Desmopressin acetate is commonly used to treat VWD and helps promote the release of additional VWF in the body. Other treatments include factor replacement therapy, antifibrinolytic drugs, and birth control pills.3
VWD is the most common bleeding disorder in girls and women. VWD is an inherited disorder characterized by low levels of or non-functional VWF protein. VWF helps with clotting, so when it is either missing or not working properly, heavy bleeding may occur which is difficult to stop.3 In women, VWD may present as heavy menstrual bleeding, or may be brought on by childbirth. Diagnosis of VWD is made through a series of clinical tests (i.e., factor VII clotting activity, VWF antigen).4
Congenital Factor VII Deficiency (cFVIId):5
- cFVIId is a rare genetic bleeding disorder caused by the deficiency or reduced activity of clotting factor VII
- cFVIId affects between 1 in 300,000 to 1 in 500,000 individuals in the general population
- cFVIId is the most common of the rare bleeding disorders
- The presentation of cFVIId is varied, as some individuals will be asymptomatic while others experience symptoms more typical of hemophilia, including bleeding in the joints and severe hematomas
- The severity of the disorder is not directly linked to the level of factor VII activity, as some individuals with relatively low levels of factor VII may be asymptomatic
- Diagnosis of cFVIId is based on identification of characteristic symptoms, detailed patient history, thorough clinical evaluation, and a variety of specialised blood tests
- Specialized blood tests include screening coagulation tests (i.e., aPTT and PT), where individuals with cFVIId should have a normal aPTT and a prolonged PT, and a factor VII assay which should demonstrate reduced factor VII activity
Glanzmann’s Thrombasthenia (GT):
- GT is a rare blood clotting disorder caused by a gene abnormality, which results in abnormal levels of alpha IIB beta 3 integrin platelet function6,7
- Globally, 1.0 per million persons are affected by GT6
- GT typically presents at birth, or shortly after, with an increased tendency to bleed and bruise7
- Epistaxis is a common manifestation of GT, along with gingival bleeding, purpura, and mennorrhagia6,8
- The severity of bleeds can vary greatly in individuals with GT; however, some people may experience severe, life-threatening hemorrhages7
- Diagnosis of GT is conducted through platelet aggregation studies and flow cytometry which can show abnormal expression of alpha IIB beta 3 integrin6
Acquired Hemophilia A (AHA):
- AHA is an acquired autoimmune disease caused by autoantibodies to FVIII, which result in FVIII deficiency and a bleeding tendency1
- 3–1.5 per million persons are affected yearly1
- AHA must be treated quickly and effectively because:
- Fatal bleeds may occur at any time until the inhibitor has been eliminated2 with up to a 22% mortality rate3
- 70% of AHA patients will experience a life-threatening bleed4
- Increased frequency in young women of childbearing age who are between 20 and 40 years old2, manifested by postpartum bleeding2
- General increase in AHA with age among men and women, especially in individuals aged 60 years and older2
- ED physicians are in a unique position to affect outcomes of AHA patients who present to the ED
- Higher awareness of AHA may lead to earlier diagnosis and improved outcomes
Overview
- Prompt triage and assessment
- Triage
- Individuals with bleeding disorders should be triaged urgently, because delays in administering factor concentrate treatment can significantly affect morbidity and mortality9
- Consultation with the patient’s hematologist or a regional hemophilia treatment center professional is strongly advised; however, this should not delay giving clotting factor replacement to the patient
- Determine the severity of the bleed
| TRIAGE10,11 | ||
|---|---|---|
| Level I | Resuscitative | |
| Level II | Emergent | Major/moderate bleeds |
| Level III | Urgent | Mild/moderate bleeds |
| Level IV | Less Urgent | |
| Level V | Non Urgent | |
- Case presentation
- Details (age, gender, etc.)
- Past medical history:
- g., Current medication
Examination
- Pulse
- Respiratory rate
- Application of any clinical tools/algorithms
- Assessment11
- Treatment for a suspected bleeding episode is based on clinical history. Physical exam findings may be normal in the early phases of most hemophilic bleeds. Spontaneous bleeding is common in individuals with severe disease (factor levels <1%). When in doubt, administer clotting factor replacement therapy immediately.
- Treatment decisions should be based on the suspicion of a bleeding-related problem, not the documentation of one.
- If the patient or the parent of a patient suspects that occult bleeding is occurring, administer clotting factor replacement. Patients often are instructed to carry with them appropriate factor replacement dosing guidelines, as advised by their treating hematologist.
Actions
Initial Management
- Treat with factor first, then investigate
| TREATMENT2 |
| ED staff should treat first, before conducting any other investigations |
| Invasive procedures, such as withdrawing blood from joint bleeds, should be delayed until patients receive the replacement blood factor |
- E.g., investigations
- No IM and no ASA
- Avoid invasive procedures (such as arterial punctures) unless the patient has factor replacement
- Contact patient’s bleeding disorder treatment centre where a hematologist is always on call
| Coagulation Disorder | BT or Closure Time |
CBC | PT/INR | aPTT |
| Hemophilia1 | Normal | Normal | Normal | Prolonged |
| Acquired Hemophilia2 | Normal | Normal | Normal | Prolonged |
| FVII Deficiency3 | Normal | Normal | Prolonged | Normal |
| Glanzmann’s Thrombasthenia4 | Prolonged | Normal | Normal | Normal |
| von Willebrand Disease4 | (Prolonged) | Normal | Normal | (Prolonged) |
Supportive Management
- E.g., transfusion therapy
Practical Considerations
- Current guidelines12 recommend that patients with rare bleeding disorders be managed by a multidisciplinary team of specialists, with expertise in treating patients with coagulation disorders1,2
- If interested, the Canadian Hemophilia Society houses a searchable directory of hemophilia treatment centers3
- Recognize that bleeding in the head, spine, abdomen, or pelvis may initially be occult and potentially life-threatening
Diagnostic Studies11
- Clotting factor replacement therapy should be given before any diagnostics studies (e.g., X-rays, CAT scans, etc.) are performed to evaluate a suspected bleeding problem, especially in the case of head trauma or suspected intracranial hemorrhage. For routine joint bleeding, no radiographic studies are indicated.
- For patients with hemophilia who have illnesses or disorders that necessitate an invasive procedure (e.g., lumbar puncture, arterial blood gas, arthrocentesis, etc.) or surgery, factor replacement therapy to 100% must be administered in the emergency department prior to the planned procedure or surgery.
- For an individual with known hemophilia, routine laboratory studies (e.g., PT, PTT, factor levels) are not indicated in the treatment of a routine bleeding episode unless requested by the patient’s hematologist. The clinical severity of a patient’s hemophilia is gauged by his or her baseline clotting factor level, a value that remains fairly constant throughout that person’s life.
Indications for Factor Replacement Therapy11
- Suspected bleeding into a joint or muscle
- Any significant injury to the head, neck, mouth, or eyes or evidence of bleeding in these areas
- Any new or unusual headache, particularly one following trauma
- Severe pain or swelling at any site
- All open wounds requiring surgical closure, wound adhesive, or steri-strips
- History of an accident or trauma that might result in internal bleeding
- Any invasive procedure or surgery
- Heavy or persistent bleeding from any site
- Gastrointestinal bleeding
- Acute fractures, dislocations, and sprains
Treatment
Hemophilia A without Inhibitor11
The treatment of choice for individuals with hemophilia A (factor VIII deficiency) is recombinant factor VIII or else the patient’s product of choice. Plasma-derived concentrate is a suitable alternative in an emergency situation when recombinant Factor VIII is not available. Cryoprecipate and fresh frozen plasma are no longer recommended for treatment of individuals with hemophilia A.
When bleeding is severe, the appropriate dose of factor VIII product should be administered to result in a factor VIII level of 80–100%.
Mild Hemophilia A with Non-Life or Limb Threatening Bleeding
Individuals with mild hemophilia A (factor VIII greater than 5%) who are experiencing non-life or limb threatening bleeding may respond to desmopressin if they have been shown to respond to this treatment previously. Otherwise, treatment is the same as for other individuals with hemophilia A.
Hemophilia B without Inhibitor
The treatment of choice for individuals with hemophilia B (factor IX deficiency) is recombinant factor IX or else the patient’s product of choice. Plasma-derived concentrate is a suitable alternative in an emergency situation when recombinant Factor IX is not available. Fresh frozen plasma is no longer recommended for treatment of individuals with hemophilia B. Note that cryoprecipitate does not contain Factor IX.
When bleeding is severe, the appropriate dose of factor IX product should be administered to result in a factor IX level of 80–100%.
cFVIId5
The treatment for individuals with cFVIId is dependent on the severity of the disease. However, specific treatment options for acute bleeds in individuals with cFVIId include recombinant factor VII, prothrombin complex concentrates, and frozen fresh plasma. Antifibrinolytics (such as aminocaproic acid) can be used to help alleviate bleeding symptoms.
Additionally, some individuals with cFVIId may undergo prophylactic therapy to minimize future bleeding complications.
GT7
Individuals with GT may require blood platelet transfusions. If blood platelet transfusions are not effective, recombinant factor VIIa can be used to treat bleeding episodes and for perioperative management.
Acronyms
ED: Emergency department
aPTT: Activated partial thromboplastin time
APCC: Activated prothrombin complex concentrate
AH: Acquired hemophilia
BU: Bethesda unit
FVIII: Factor VIII
FIX: Factor IX
HTC: Hemophilia treatment centre
ITI: Immune tolerance induction
IU: International unit
PT : prothrombin time
rFVIIa: Recombinant activated factor VII
VWF: von Willebrand factor
References
- Centers for Disease Control. What is Hemophilia? 2020. Available at: https://www.cdc.gov/ncbddd/hemophilia/facts.html. Retrieved November 10, 2020.
- Winikoff R. Symptomatic Carriers of Hemophilia. All About Hemophilia: A Guide for Families. https://www.hemophilia.ca/files/Chapter%2014.pdf
- Centers for Disease Control. What is von Willebrand Disease? 2020. Available at: https://www.cdc.gov/ncbddd/vwd/facts.html#:~:text=Von%20Willebrand%20disease%20(VWD)%20is,von%20Willebrand%20factor%20(VWF). Retrieved November 10, 2020.
- Centers for Disease Control. Von Willebrand Disease Diagnosis. 2020. Available at: https://www.cdc.gov/ncbddd/vwd/diagnosis.html. Retrieved November 10, 2020.
- National Organization for Rare Disorders. Factor VII Deficiency. 2018. Available at: https://rarediseases.org/rare-diseases/factor-vii-deficiency/. Retrieved November 10, 2020.
- Krause KA, et al. Glanzmann Thrombasthenia. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2020, StatPearls Publishing LLC.; 2020.
- National Organization for Rare Disorders. Glanzmann Thrombasthenia. Available at: https://rarediseases.org/rare-diseases/glanzmann-thrombasthenia/. Retrieved November 10, 2020.
- Yadalam U, et al. Periodontal considerations for Glanzmann’s thrombasthenic patient. Journal of Indian Society of Periodontology. 2008;12(1):26-27.
- Guidelines for Emergency Department Management of Individuals with Hemophilia and Other Bleeding Disorders. National Hemophilia Foundation. 2014. Available at: https://www.hemophilia.org/Researchers-Healthcare-Providers/Medical-and-Scientific-Advisory-Council-MASAC/MASAC-Recommendations/Guidelines-for-Emergency-Department-Management-of-Individuals-with-Hemophilia. Retrieved February 9, 2018.
- Canadian Hemophilia Society. Emergency Care. Available at: https://www.hemophilia.ca/emergency. Retrieved November 10, 2020.
- Bullard MJ, et al. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) Guidelines 2016. CJEM. 2017;19(S2):S18-S27.
- Srivastava A, et al. WFH Guidelines for the Management of Hemophilia, 3rd edition. Haemophilia. 2020;26 Suppl 6:1-158.
Acquired Hemophilia A #1
- 77 y/o female presents with a painful buttock bruise.
- Lost her footing after getting out of the shower and tripped over the bathroom counter, immediately painful.
- Wasn’t sure about coming into hospital but bruise seemed large.
- May have taken ASA 2 days earlier for headache.
- No history of bleeding tendencies.
- Examination
- Actions
Initial Visit:
NIDDM
- HTN
- Dyslipidemia
- Medications: metformin, Ramipril
- Allergies: NKA
- Tried ASA for primary prevention years earlier – didn’t like skin effects
- O/E
- VS Normal
- Large 15 X 20cm buttock hematoma, superficial, no collection. No other bleeding stigmata.
Return Visit (Day 2)
- Hematoma has grown, extensive bruising involving entire buttock and tracking down thigh to lower leg, increasingly painful.
- Exam now shows large fluctuant hematoma. Rest of exam normal.
- Labs: PT/INR, CBC normal, Hgb: 120
Initial Management:
Traumatic hematoma => expectant management. F/u as needed
Return Visit Management
- Hematoma evaluation performed with 150 cc removed through 5cm incision, loose packing and dressing applied.
- Rushed back to hospital 6 hours later due to presyncopal symptoms and worsening buttock pain. Dressing soaked through completely.
- Pale, slightly diaphoretic, anxious.
- O/E Wound continues to ooze with impressive flow.
- Surgical packing and pressure dressing applied.
- Tranexamic acid IV given.
- Blood loss diminished now but still ongoing.
- Severe pain with hip flexion and contraction of gluteus muscle (unable to stand up from chair).
- Hgb 90
- PT/ INR normal
- PTT 78sec
Practice Considerations
Acquired hemophilia is a rare but potentially life-threatening bleeding disorder caused by the development of autoantibodies (inhibitors) directed against plasma coagulation factors, most frequently factor VIII (FVIII).
AHA should thus be considered in the differential diagnosis particularly in postpartum women and the elderly with new bleeding tendency or prolonged activated partial thromboplastin time who have no prior personal or family history of bleeding.
In approximately 50% of AHA patients, especially elderly patients, autoantibody development against factor VIII is idiopathic [2, 26, 27], indicating that the acquired inhibitors develop via an autoimmune mechanism.
Treatment
During acute bleeding episodes, effective control of bleeding manifestations is the primary objective. However, the ultimate therapeutic goal is to eliminate the inhibitor and cure the disease. Hemostatic therapy with bypassing agents should be provided. Immune tolerance induction therapy has shown poor efficacy in treating AHA. Immunosuppressive treatment should thus be initiated to eradicate inhibitors as soon as the diagnosis of AHA is confirmed.
Hemophilia with Care Plan #2
23 y/o male presents with right sided abdominal and groin pain
Pain started several hours after jumping on a trampoline with his friends
He tells you he has hemophilia B
- Examination
- Actions
Temperature 37.7oC
Pulse 115
BP 110/65
Appears very uncomfortable. Unable to stand up straight or lie completely flat on exam bed due to pain
Keeps both hips and knees in flexed position
Reports “pins and needles” with altered sensation to anterolateral right thigh
Guarding on palpation, no mass
No swelling, warmth or bruising to abdomen or over groin
Initially bloodwork: Hgb 117, plts 400, WBC 14.3, INR 1.2, aPTT 76sec
Initial Management:
Possible bleed must be on the differential given underlying hemophilia
Confirm the type and severity of hemophilia and if bleeding is suspected, always treat first before initiating investigations/imaging
This patient has a Factor First card stating he has severe hemophilia B (FIX level < 1%) and should receive recombinant factor IX (rFIX) concentrate for bleeding
Per the patient treatment protocol, he is given rFIX concentrate 110U/kg IV push for suspected major bleeding
Differential diagnoses at this point could include:
Pulled groin muscle
Hip joint bleed
Iliopsoas muscle bleed
Appendicitis
Renal colic
He is sent for CT abdo/pelvis that reveals a large right iliopsoas bleed
Practice Considerations
Hemophilia A and B are X-linked congenital bleeding disorders that occur due to deficiency in FVIII or FIX clotting factors respectively
Hemophilia is classified based on severity of the clotting factor deficiency. Factor levels < 1% (<0.01U/ml) is considered severe disease, factor levels 1-5% (0.01 – 0.05U/mL) is moderate, and factor levels > 5% to 40% (>0.04 – 0.40U/mL) is mild
Bleeding tendency correlates with degree of clotting factor deficiency and those with severe hemophilia can present with spontaneous as well as trauma-associated bleeding
Severe hemophilia patients may be on prophylaxis treatment with regular clotting factor infusions to prevent/protect against spontaneous bleeding
Timely evaluation and treatment of suspected bleeding is critical in hemophilia and patients should always be given clotting factor concentrate as soon as possible to prevent complications of uncontrolled bleeding (i.e. “treat first” or “factor first”).
All hemophilia patients should be managed and followed by a comprehensive care hemophilia treatment centre (HTC). In Canada, hemophilia patients should be included in the national registry and all HTC-associated hemophilia patients should carry with them a “Factor First” card which states their diagnosis and treatment protocol for emergency bleeding.
Treatment
Iliopsoas bleeds:
Do not miss this bleed!
High morbidity and potentially life-threatening
Requires aggressive treatment
Physiotherapy is very important because inflammation from bleeding can cause fibrosis and muscle contracture
Muscle dysfunction – high risk of re-bleeding
May be misdiagnosed because pain can mimic
Appendicitis
Renal colic
Hip bleed
Hip or lower back arthritis
Often no bruising or swelling superficially (deep muscle bleed)
There may not be a drop in Hgb initially
Exam findings
Patient walks with limp, on toe, knee bent
Pain in along iliopsoas bursitis distribution
Groin
Back
Front of the leg
Hip flexion contracture – unable to extend on affected side without arching the lower back
Maneuvers that stretch the iliopsoas causes pain
Red flags!
If the patient complains of numbness, tingling, or pins and needles sensation
If there is weakness on knee extension
Suggests vessel or femoral nerve compromise
Femoral nerve or vessels have been compressed or damaged
Requires immediate attention
replay
Von Willebrand Disease (VWD) #3
31-year-old female G1P1 presents with heavy vaginal bleeding 6 days post-partum following an uncomplicated spontaneous vaginal delivery.
Her flow has increased significantly over the past 24 hours. She has soaked through several heavy absorbency pads and is now using a towel.
Past medical history:
She tells you she has von Willebrand’s disease.
In the past she has had problems with:
Epistaxis requiring cautery
Excessive bleeding for 4 days after wisdom teeth extraction
Heavy menstrual bleeding
Received DDAVP prior to lumpectomy for a benign breast lesion
She did not require DDAVP or VWF concentrate with her delivery as third trimester VWF levels were above 75% (i.e. normalized)
Her only medications are pregnancy multivitamins and tranexamic acid that were prescribed by her hematologist to take for 14 days post-partum
Her Factor First card states she should receive DDAVP for bleeding
- Examination
- Actions
- Temperature 37.1oC
- Pulse 115 bpm
- BP 100/65
- She appears pale
- Gyne exam – firm uterus with fundus below umbilicus, bright red blood and 5cm clots in the vagina
Initial Management:
- Supportive management
- Investigations:
- CBC, type & screen, lytes, creatinine, INR, PTT, fibrinogen
- VWF levels (VWF:Ag, VWF:RiCoF activity, and FVIII activity) sent but will not return for a few days
- Old chart and hematologist notes reports type 1 VWD with baseline VWF:Ag 0.28 U/mL (28%), VWF:RiCof activity 0.26 U/mL (26%), FVIII activity 0.41 U/mL (41%)
Results and Supportive Management
- Her bloodwork returns showing normal platelet and WBC count. Hemoglobin is 87.
- Creatinine, electrolytes, and INR are normal.
- aPTT is elevated at 38 seconds (can be seen when VWF and FVIII levels are low)
Treatment
- The patient was given a dose of DDAVP 0.3mcg/kg subcutaneously followed by a second dose 24 hours later. VWF levels were re-sent after the second DDAVP dose and she was sent home on tranexamic acid
- 2 days later she returns to ED with recurrent heavy vaginal bleeding.
- A third dose of DDAVP is given.
- The post-second DDAVP dose VWF levels returned showing normal levels [VWF:Ag 1.13 U/mL (113%), VWF:RiCof 1.08 U/mL (108%), FVIII activity 1.50 U/mL (150%)]
- Continued bleeding with normal VWF levels should prompt investigations for other causes of bleeding (e.g. anatomic
- Gynecology is consulted and retained products/placenta evacuated from the uterus
Practice Considerations
- VWD is the most common congenital bleeding disorder with a prevalence of 1:100 to 1:1000
- Bleeding symptoms can vary depending on severity and type of VWD
- Bleeding symptoms are commonly mucocutaneous (e.g. epistaxis, gingival, gastrointestinal, genitourinary, uterine/menorrhagia) and can occur with invasive procedures (dental extractions, surgery) and childbirth.
- Bleeding assessment tools (BATs) are helpful for objective evaluation of bleeding symptoms and should be used in the work up of possible VWD or bleeding disorders. (E.g. ISTH BAT, condensed MCMDM-1 VWD score – these scoring tools can be found on the WFH website).
- DDAVP increases endogenous release of VWF multimers from endothelial cells and is effective treatment in type 1 and some type 2 VWD. However, DDAVP testing for response prior to treatment is recommended as not all VWD patients have an adequate response to DDAVP.
- DDAVP can cause symptomatic hyponatremia especially in young children and elderly. Electrolytes should be monitored with repeated dosing (especially if given more frequently than q 24 hours) and patients should restrict fluids to ≤ 1500mL for 24 hours after DDAVP
- In those where DDAVP response is inadequate or unknown, VWF concentrate (e.g. Humate P, Wilate) is recommended
- Tachyphylaxis can occur with repeated DDAVP dosing given within a short interval (e.g. < 24 hours). Hematology should be consulted if initial doses are ineffective or more than 2 consecutive doses of DDAVP have been given.
- Use of antifibrinolytics (e.g. tranexamic acid) either alone in mild mucosal bleeding or as an adjunct to DDAVP or VWF concentrate for more severe mucosal bleeding is recommended.
- DDAVP may be given subcutaneously or IV (in 50cc saline infused over 30mins) at a dose of 0.3mcg/kg
- It can also be administered intranasally as 150mcg/metered dose nasal spray, 2 sprays for adults, 1 spray if <40kg. Intranasal DDAVP dose for VWD should not be confused with the dose used for nocturnal enuresis (10mcg/spray).
- VWF and FVIII levels increase during pregnancy and can also increase during a stress response
- If levels normalize in the third trimester (VWF:RiCof activity >0.50U/mL, 50%), usually no primary hemostatic prophylaxis is given for labor and delivery.
- Delayed post-partum bleeding can occur when VWF levels fall back to normal usually within the first week post-partum.
- Post-partum bleeding is reported in 20-25% of VWD women (vs. 1.3% in the normal population).
- Tranexamic acid prescribed for 14 days post-partum is usually effective at preventing this however more significant bleeding may still occur.
- DDAVP or VWF concentrate maybe required to control bleeding.
- If there is continued bleeding despite adequate VWD treatment (I.e. normal VWF levels), then other causes of bleeding (anatomical, retained products of conception) must be considered.
VWD Case – Meningitis needing LP #4
- 21-year-old female presents with severe headache, neck stiffness, photophobia and fever
- You are concerned about meningitis and would like to do a lumbar puncture for diagnosis
- Past medical history:
- She tells you she has von Willebrand’s disease.
- In the past she has had problems with:
- Epistaxis requiring cautery
- Excessive bleeding for 4 days after wisdom teeth extraction
- Heavy menstrual bleeding
- She does not have a medical alert bracelet or a Factor First Card on her.
- She does not recall what type of von Willebrand’s disease she has and has never been treated with DDAVP before.
- Examination
- Actions
- Temperature 38.9oC
- Pulse 105
- Respiratory rate: 24
- She lies on her side, curled in the fetal position and demonstrates signs of nuchal rigidity
- Several quarter sized bruises on her lower extremities, no petechiae
- Chest is clear, abdominal exam is benign
Initial Management:
- Fluids and Tylenol as needed to treat fever
- Investigations:
- CBC, lytes, Creatinine, PTT, INR, blood cultures
- VWD studies: VWF:Ag, VWF:RCoF activity, FVIII level
- If there is no documentation of her baseline VWF levels or diagnosis, VWF levels should ideally be sent before initiating any treatment.
- However, the turn-around-time for VWD studies is generally between 1-2 days up to a couple of weeks depending on your local hemostasis laboratory and availability of testing.
- Decision for treatment in an urgent setting (bleeding, procedural intervention) must be made without these results.
Results and Supportive Management
- Her bloodwork returns showing normal hemoglobin and platelet levels. WBC is slightly elevated at 14.1.
- Creatinine, electrolytes, and INR are normal.
- aPTT is elevated at 40 seconds.
Treatment
- Treat as per usual the suspected meningitis with antibiotics before the lumbar puncture.
- In this case where the baseline VWF levels and response to DDAVP is unknown, VWF concentrate should be given prior to an invasive procedure such as a lumbar puncture.
- The aPTT is elevated on the baseline bloodwork which suggests VWF and FVIII levels <0.30 U/mL (30%).
- For lumbar punctures where there is a concern for epidural bleeding, targeting VWF and FVIII levels of >0.50U/mL (50%) is recommended.
- The recommended dose for VWF concentrate for severe bleeding or prior to invasive procedure is 60 RiCof units/kg IV.
Practice Considerations
- VWD is the most common congenital bleeding disorder with a prevalence of 1:100 to 1:1000
- Bleeding symptoms can vary depending on severity and type of VWD
- Bleeding symptoms are commonly mucocutaneous (e.g. epistaxis, gingival, gastrointestinal, genitourinary, uterine/menorrhagia) and can occur with invasive procedures (dental extractions, surgery) and childbirth.
- Bleeding assessment tools (BATs) are helpful for objective evaluation of bleeding symptoms and should be used in the work up of possible VWD or bleeding disorders. (E.g. ISTH BAT, condensed MCMDM-1 VWD score – these scoring tools can be found on the WFH website).
- DDAVP increases endogenous release of VWF multimers from endothelial cells and is effective treatment in type 1 and some type 2 VWD. However, DDAVP testing for response prior to treatment is recommended as not all VWD patients have an adequate response to DDAVP.
- DDAVP can cause symptomatic hyponatremia especially in young children and elderly. Electrolytes should be monitored with repeated dosing (especially if given more frequently than q 24 hours) and patients should restrict fluids to ≤ 1500mL for 24 hours after DDAVP.
- In those where DDAVP response is inadequate or unknown, VWF concentrate (e.g. Humate P, Wilate) is recommended.
- Tachyphylaxis can occur with repeated DDAVP dosing. Hematology should be consulted if initial doses are ineffective or more than 2 consecutive doses of DDAVP have been given.
- Use of antifibrinolytics (e.g. tranexamic acid) either alone in mild mucosal bleeding or as an adjunct to DDAVP or VWF concentrate for more severe mucosal bleeding is recommended.
- DDAVP may be given subcutaneously or IV (in 50cc saline infused over 30mins) at a dose of 0.3mcg/kg.
- It can also be administered intranasally as 150mcg/metered dose nasal spray, 2 sprays for adults, 1 spray if <40kg. Intranasal DDAVP dose for VWD should not be confused with the dose used for nocturnal enuresis (10mcg/spray).
Glanzmann’s Thrombasthenia #5
- 5-year-old male with bleeding at the site of an empty tooth socket
- The patient shed his first deciduous tooth and has experienced gingival hemorrhage for 2 days since
- The patient’s mother reports that the child has previously experienced repeated episodes of epistaxis and has received a blood transfusion to control bleeding
- Previous laboratory tests have revealed normal platelet counts
- Examination
- Actions
- Compression of the socket was unsuccessful in stopping the hemorrhage
- Laboratory tests ordered:1,2
- Platelet count = 300,000/mm3 (normal)
- Hemoglobin = 12.0 g/dL (normal)
- PT = 10 seconds (normal)
- aPTT = 45 seconds (normal)
- Bleeding time = 15 minutes (prolonged)
Initial Treatment
- The patient received a platelet transfusion to stabilize the hemorrhage
- Upon analyzing the laboratory results, the patient was determined to have Glanzmann’s thrombasthenia (GT) and was initiated on 90 µg/kg NiaStase RT® (rFVIIa) q4hrs
Treatment of GT
- Platelet transfusions may be required in individuals with GT. With repeated platelet transfusions, patients may develop antibodies, which hinder the benefit of future transfusions3
- Factor replacement therapies (e.g., NiaStase RT®) are used to treat bleeding episodes in people living with GT and for the perioperative management of bleeds3
- Additional treatments may be used to manage symptoms of GT, such as antifibrinolytic agents
Practical Considerations
- GT is a rare, autosomal recessive blood clotting disorder caused by a gene abnormality, which results in abnormal levels of alpha IIB beta 3 integrin platelet function3,4
- Globally, 1.0 per million persons are affected by GT4
- GT typically presents at birth, or shortly after, with an increased tendency to bleed and bruise3
- Epistaxis is a common manifestation of GT, along with gingival bleeding, purpura, and mennorrhagia4,5
- The severity of bleeds can vary greatly in individuals with GT; however, some people may experience severe, life-threatening hemorrhages3
Female Hemophilia B Carrier #6
- 48-year-old female presents with menorrhagia and abdominal pain
- The patient reports experiencing menorrhagia for the past 5 years and that she has previously been treated for an ovarian cyst
- The patient is not currently taking hormonal birth control
- Examination
- Actions
- Ultrasound and physical exam revealed no ovarian cysts or signs of endometriosis
- Laboratory tests
- PT = 9 seconds (normal)
- aPTT = 50 seconds (prolonged)
- Factor VIII = 98% of normal
- Factor IX = 37% of normal (mild deficiency)
- Liver function test = normal
Initial Treatment
- Acetominophen was administered to treat abdominal pain
- Ovarian cysts and other gynecological explanations for menorrhagia were ruled out
- Laboratory results revealed a decificiency in factor IX (37% FIX activity)
- Patient was started on tranexamic acid 4 g qd to control her menorrhagia6
Practical Considerations7
- Although bleeding disorders may be perceived as male-only diseases, women are also affected by them
- Women can have lower than normal plasma levels of factor VIII or IX, and thus may exhibit symptoms of hemophilia depending on their residual factor activity
- Gynecological and obstetrical bleeding (e.g., menorrhagia, dysmenorrhea, metrorrhagia) may be symptoms of a bleeding disorder in women and should be investigated
Treatment of Women’s Rare Bleeding Disorders7
- Mennorhagia may be treated with hormonal oral contraceptives (estrogen and progestin) or a levonorgestrel intrauterine device (e.g., Mirerna® IUS)
- Use of ibuprofen to treat dysmennorrhea should be avoided as it will increase bleeding; however, acetominophen may be administered
- Antifibrinolytic agents may be used to treat bleeding symptoms
- Various FIX products with either standard half-life (SHL) or extended half-life (EHL) may be used in a surgical setting to maintain the desired level of factor
- In women with lower levels of residual FIX activity and more severe symptoms of factor IX deficiency, recombinant factor IX products may be used as treatment
Congenital Factor VII Deficiency #7
- 18-year-old male presents with extensive bleeding from the site of appendectomy
- Family history of severe bleeding in siblings
- Consanguinous parents
- Recent refugee and never investigated in his country of birth
- This was the patient’s first surgery
- History of chronic epistaxis
- Examination
- Actions
- Temperature = 37.9 °C
- Examination revealed moderate hematomas on the patients abdomen
- Laboratory tests1
- PT = 20 seconds (prolonged)
- aPTT = 28 seconds (normal)
- Factor VII levels = 20%
Initial Treatment
- The patient was started on acetaminophen and i.v. fluids to control the fever
- Bleeding was controlled with a compress
- Reduced Factor VII levels and prolonged PT support a diagnosis of congenital factor VII deficiency (cFVIId)
- Upon diagnosis of cFVIId, the patient was started on 15 µg/kg NiaStase RT®; bleeding was stabilized with a single dose
Treatment of cFVIId8
- Treatment for cFVIId varies greatly depending on the severity of the symptoms and the patient’s existing health at the time of diagnosis (e.g., presence of co-morbidities)
- Acute bleeds can be treated with recombinant factor VII (rFVIIa) or plasma derived FVII
- Bleeding symptoms may be addressed with antifibrinolytic agents
Practical Considerations8
- cFVIId is a rare, autosomal recessive, genetic bleeding disorder caused by the deficiency or reduced activity of clotting factor VII (FVII)
- cFVIId affects between 1 in 300,000 to 1 in 500,000 individuals in the general population
- The presentation of cFVIId is varied, as some individuals will not show any symptoms (asymptomatic), while others experience symptoms more typical of hemophilia, including bleeding in the joints and severe hematomas
- The severity of the disorder is not directly linked to the level of factor VII activity, as some individuals with relatively low levels of factor VII may be asymptomatic
References:
- Kamal AH, et al. How to Interpret and Pursue an Abnormal Prothrombin Time, Activated Partial Thromboplastin Time, and Bleeding Time in Adults. Mayo Clin Proc. . 2007;82(7):864-873.
- Russeau AP, et al. Bleeding Time. StatPearls. Treasure Island (FL): StatPearls Publishing. Copyright © 2020, StatPearls Publishing LLC.; 2020.
- National Organization for Rare Disorders. Glanzmann Thrombasthenia. Available at: https://rarediseases.org/rare-diseases/glanzmann-thrombasthenia/. Retrieved November 10, 2020.
- Krause KA, et al. Glanzmann Thrombasthenia. StatPearls. Treasure Island (FL): StatPearls Publishing. Copyright © 2020, StatPearls Publishing LLC.; 2020.
- Yadalam U, et al. Periodontal considerations for Glanzmann’s thrombasthenic patient. Journal of Indian Society of Periodontology. 2008;12(1):26-27.
- Leminen H, et al. Tranexamic acid for the treatment of heavy menstrual bleeding: efficacy and safety. International journal of women’s health. 2012;4:413-421.
- Winikoff R. Symptomatic Carriers of Hemophilia. All About Hemophilia: A Guide for Families.
- National Organization for Rare Disorders. Factor VII Deficiency. 2018. Available at: https://rarediseases.org/rare-diseases/factor-vii-deficiency/. Retrieved November 10, 2020.
Disclaimer
CAEP Notes includes clinical tools and resources intended for use by healthcare professionals. These tools do not give professional advice; physicians and other healthcare professionals who use these tools or databases should exercise their own clinical judgment as to the information they provide. The contents of the CAEP Notes tool, such as text, graphics and images are for informational purposes only. While information on this site has been obtained from sources believed to be reliable, CAEP and its partners do not warrant the accuracy of the information contained on this site.
